Episode 10 – Parts 1 & 2
Part 1
Published on Wednesday, December 21, 2016
In part one of this two-part podcast, host Adam Siladi chats via Skype with John Lynn from healthcarescene.com about how providers are stepping up their patient engagement efforts, largely because today’s healthcare consumers demand more tools for taking charge of their own health.
Part 2
Published on Wednesday, December 21, 2016
In part two of this two-part podcast, host Adam Siladi continues his Skype conversation with John Lynn from healthcarescene.com. They explore how providers are using patient engagement tools to help forge true partnerships in health between providers and today’s informed, engaged healthcare consumers.
“Imagine this: Let’s actually communicate with the patient. I think that’s largely going to happen through the Patient Portal, but we’re also seeing it through secure text message, we’re also seeing it through telemedicine, even through mobile apps.”
John Lynn, blogger for Healthcarescene.com
Topics from this episode
A world of apps and trackers
Patients and practices alike have embraced apps and trackers because they are efficient, low-cost, and effective methods for creating true healthcare partnerships. But beyond the technology, such tools are effective because they help providers gain a deeper understanding of each patient’s needs. The healow family of apps can handle all the basics — from online booking, personal health records, and lab results, to reminders, secure messaging, and TeleVisits. But these apps are also customizable for each practice’s priorities and approach to patient engagement. With proper training, healow can become a truly interactive platform, helping ensure providers and patients discover the key issues that must be addressed with each case and plan an effective course of treatment to ensure optimal health.

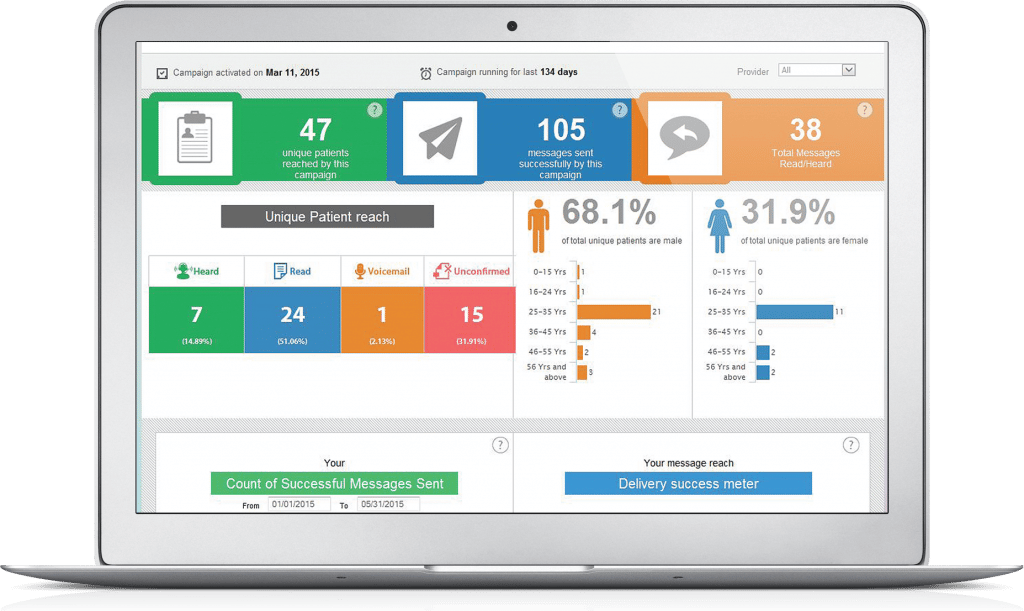
Efficiency, data, and engagement
At one level, Electronic Health Records simply speed up patient engagement campaigns — issuing reminders and saving time and trouble — without changing how medicine works. But engagement is about more than speed. It’s about overcoming providers’ concerns about messaging, apps and telemedicine, and showing them that such tools can make practices more efficient. And tools such as ClinicalWorks Messenger can do still more, helping harness the wealth of data practices generate, identifying which patients will benefit from which kinds of campaigns, and helping guide practices toward the best ways to reach out to those patients.
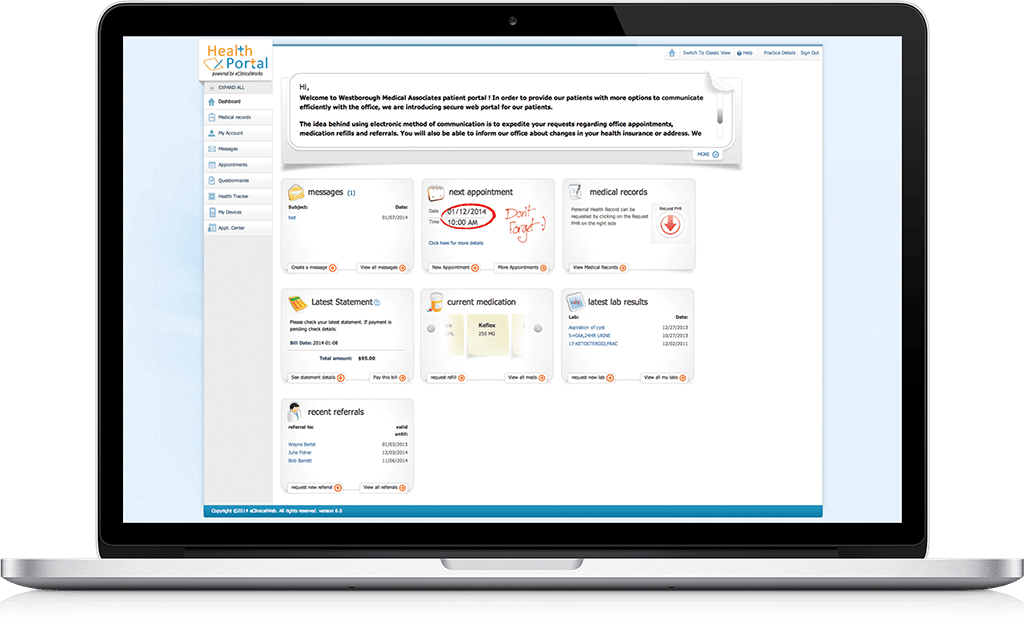
Patient Portal
As medicine shifts to value-based payment models, engagement tools such as the eClinicalWorks Patient Portal are more valuable than ever. Patients enjoy 24/7 access to their medical records, lab records, and messages. However, as you’ll hear in our Skype podcast, Portal is best seen as neither a novelty nor a luxury. Online tools today provide all patients, from the tech-savvy to those still learning about computers, with the tools they will need to take full charge of their health. Moreover, those tools are just the beginning. To make the most impact on healthcare, providers must then engage their patients through ongoing communications.
Part 1
Adam: I’m Adam Siladi with the eClinicalWorks podcast. Now, the healthcare industry is always changing, so to stay on top of that, we decided to speak with John from healthcarescene.com, which is a collection of blogs, talking about all things with the healthcare industry, in general. So, stay tuned for our interview – it’s going to be a two-part interview, so after this portion, be sure to stay tuned. Take a look.
Adam: John, thanks for being here, tell us a little bit about healthcarescene.com.
John: Sure, so healthcarescene.com is a network of about 10 healthcare IT blogs that we’ve created over the last 11 years. We actually are approaching 11,000 blog posts over 11 years, so we’ve created a lot of content over that time period. Along with that, we also, we create great healthcare IT content for sure, but then along with that, we’ve also expanded to doing careers at healthcare IT central. So we have a full job port there, for those who are interested in the healthcare IT career space, and then three years ago we launched the Healthcare IT marketing and PR conference, which you can find the conference in the community at HITMC.com, which really focuses on how do we get these great technologies, these great solutions out to healthcare. So they’re getting in the hands of the people and we actually improve healthcare, because so many people have great solutions and a lot of people don’t know about it, so we need to get the word out. So that’s really the Health IT Marketing Conference and all synergists typically works around at Healthcarescene.com.
Adam: So John, one topic being talked about today is the doctor patient relationship and there are lots of efforts to strengthen that relationship, in the case of Patient-Centered Medical Home, to modernize it with electronic access and using telemedicine and wearable devices, and things like that. What’s the prevailing opinion that you’ve seen on patient engagement?
John: Well, I think the challenge is that there’s two ways to look at patient engagement. For the one perspective you have the regulatory compliance version of patient engagement which we largely call Meaningful Use, and I think that most providers and most patients don’t consider that very meaningful, so there hasn’t been a huge uptick in adoption – certainly they did enough to meet the Meaningful Use requirements, but it didn’t really change the physician-patient relationship in any meaningful way. So, unfortunately that’s what the regulations required, so they did it. I think going beyond that, we’re seeing a transformation of what patients want from their doctors, and what doctors provide the patient. This is being influenced by a number of factors. The leading one is largely is patients are paying for more of their healthcare through high-deductible plans, through their employer not covering everything that they need to, and so the patients being more responsible for their care, and as the patient becomes more responsible for their care, they start to care what interaction they have with their doctor. And piggybacking off of those other movements such as the direct primary care, the concierge model which is becoming very popular, and also we see the telemedicine which is extremely convenient for patients, we all want to do that. Who wants to drag their children into the pediatrician to see the doctor? It’s a miserable experience and telemedicine is way better for that. The problem with that is for many doctors, it doesn’t change their experience at all, and they’re still spending more or less the same time with the patient. So on the patient side it’s a huge benefit, on the doctor’s side, it’s a challenging benefit and in many cases it doesn’t get reimbursed, although we’re seeing changes around that, as well. At the end of the day, doctors want meaningful engagement with patients; patients are starting to demand it, and it’s going to go well beyond what the compliance requirements are.
Adam: So it sounds like something that both sides want, but there are some external pressures that maybe make that a little frustrating at the time that we find ourselves in now. We’ll get into that a little bit more about the payoffs, and things like that we’ve seen and that you’ve seen — but let’s talk about some of those capabilities. What do you think are some defining capabilities of patient engagement today and in the future?
John: I think there’s a whole suite of capabilities that are going to need to be addressed in order to make this happen. In fact, in the accountable care world, the value-based reimbursement world, you’re going to have to create a whole suite of capabilities. Certainly, it starts with the patient portal and giving them access to patient records – that’s almost a de facto minimum. Like can you give the records to the patient, that’s one way to engage them, so that they can see the patient, we know the famous people like e-patient Dave that showed that having access to your records can actually improve the care because the patient is the best quality control for the patient record, and they can ensure that the record is highly accurate. So we need to make those available to the patient as the first step, so that they can inform the provider of what’s accurate, what’s inaccurate, what needs to be updated, or any other changes that may have occurred, even outside of that organization. So I think that’s a minimal baseline, let’s give patients access to their record, and let them have the opportunity to update the record or at least inform the clinical organization of what needs to be changed. Then going beyond that is actually communicating with them. Imagine this: Let’s actually communicate with the patient. In the fee-for-service world, it actually makes sense why the doctor doesn’t want to over communicate with the patient — they don’t get paid for it, right? In this new value-based reimbursement world, the doctor will need that connection to the patient, in order to ensure that they are healthy, that they are compliant with whatever care plan they created with them. So I think that’s going to push us to want doctors to interact with the patients and vice versa, right? So there is that deep connection and ongoing effort to improve the care of their patient. I think that’s largely going to happen through the patient portal as well, but we’re also seeing it through secure text message, we’re also seeing it through telemedicine, even through mobile apps. You know, I think there are some interesting mobile apps that are going there that allow patients to get answers to their questions.
Adam: It’s interesting you mention all those capabilities, John, because eClinicalWorks basically offers all of those things, and we’re certainly happy to talk to people about more information if they’re looking for it. You bring up an interesting fact when you say it’s definitely going to be a bigger part and a more desirable part of a value-based system, but I think it’s also kind of valuable here in the fee-for-service. You mentioned that they’re not reimbursed for it, so if they have to return patient calls, or answer patient questions, which I think a lot of doctors feel morally obligated, if not, actually contractually or lawfully obligated to do. If they’re doing those things, getting on the phone and spending all that time on patients — if they could find a more time efficient way to do all of those things, they’re actually kind of saving themselves some money. We’ve had that said to us by some people that we’ve interviewed for the podcast, that they’ve saved tons of time, it’s more convenient, they don’t have to spend quite so much time to communicate with the patient, but they have the same effectiveness when they use those electronic-based methods.
John: That’s an interesting point, and the challenge here is this: most doctors are afraid of what it means to start communicating that way, through a patient portal, through a secure messaging system, and so there’s this fear that makes them say “Oh, I think that will be worse” or “I think I’m gonna end up giving a bunch of uncompensated care if I start using these tools.” And it turns out, the reality is totally different. My favorite example of this, is a guy named Dr. C.T. Lynn out of Colorado, he did a study on this and he did the research on it, and he literally wanted to implement a program where the patients can interact with the doctors and they could access their patient records through the patient portal. And Dr. Lynn actually took it to the doctors, and one doctor said this, which is super-fascinating. He said: ‘I’m only going to let you do this because I know you’re going to fail so badly that you will realize how bad of an idea this is and how awful this is going to be, right?’ So the doctor literally was so afraid of it and he was like ‘Yeah, I’m only going to let you do it because I think you have research vigor, and so you’re going to do it in a proper way, and you’re going to realize this is an awful idea!” And Dr. Lynn always replies ‘OK, thank you. We’ll do ahead and we’ll do it.’ And they did it, and this doctor discovered he was wrong, it actually wasn’t a huge overhead on his time and his effort, but instead it was actually a savings for him, and the doctor came back to him and apologized and essentially said ‘You were right. This is better, and I’m glad we did it.’
Adam: There’s understandably some anxiety there. I mean, you mentioned before the very first thing is giving patient portal access, and there’s some doctors who don’t even want to do that. We’ve seen doctors who’ve turned on the portal for the first time for their patients, but there’s almost nothing there because they don’t want to publish the labs, they don’t want to make it possible to request refills — they think, like you said, there will be an administrative headache. Then, the people that we’ve talked to, have found almost the opposite. But that’s really interesting, he almost challenged him to say ‘I think you’re going to find it’s terrible,’ but instead he found it the opposite.
John: Yeah, I mean what you highlighted is the problem with the portal. Everyone’s like ‘No one uses our portal.’ But it’s like ‘You didn’t put anything useful on your portal.’ So if you don’t put anything useful on your portal, no one’s going to use it, but there’s also the other problem – I went to my pediatrician, I have four children, and I said ‘Hey can I get access to your patient portal?’ Which I knew they had because they had done Meaningful Use, like I knew that they had one – the front desk person was like, ‘I’m not sure, I’ve never had that question. Hold on.’ She ran back to the practice manager, she came back to me and said, ‘Yeah we’ll email you access to it.’ Six months later, no access to it. So I even want it, I want to test it, obviously I’m a little biased because I’m a blogger, but they didn’t even know anything about it. So there’s a big learning curve that still needs to happen.
Adam: Well, I think so. I think that you hit the point there that, when we talk about engagement, engagement is a two-way street. It’s not just patients being engaged or responding to these things, but it’s also the office — the office needs to make sure that they’re educated, make sure that they’re putting the message out there because it sounds like, in your case, they have this capability, and like you said, you were an informed consumer. Little did they know you’re an informed and an involved guy, but they weren’t prepared to handle even the request to put you on the patient portal, because someone didn’t tell that front office person that that might be something that they’re doing. So I think it really highlights the fact that to be successful with patient engagement — and again, I know I keep plugging our podcast here — but we had an episode where we talked with a practice — actually I think it was in Carson City, Nevada, not too long ago — and they mentioned all of the communication that they did with their patients, and internal communication as well, that helped make them so successful.
John: Yeah, I mean, when you talk about care coordination, there’s a similar issue there. It’s communicating between providers and then also to the patient. I think that’s a challenge that needs to be done, it needs to be accomplished. No doubt, you have to have both sides engaged, that’s the real problem. There’s a lot of doctors and other providers that are afraid, and quite frankly, there’s not a lot of patients that care either. So there’s a big challenge there, as well.
Adam: That was part one of our interview with John Lynn from healthcarescene.com. Stay tuned for the next episode, and also check out our other episodes on iTunes, YouTube and my.eclinicalworks.com. For the eClinicalWorks podcast, I’m Adam Siladi, thanks for watching.
Part 2:
Adam: I’m Adam Siladi with the eClinicalWorks Podcast and this is Part two of our interview with John Lynn from healthcarescene.com, a collection of blogs that cover the healthcare industry. So, take a look at the conclusion of our interview.
Adam: Yeah, like you said, it’s a two-way street. Sometimes the patients just don’t want that type of engagement, but I think that leads me to a question of once we get patient engagement going, and we should discuss some examples that we’ve seen when it’s work, and that kind of stuff to prove our point, but I think we’re starting to touch on the fact that patient engagement almost needs to be tailored for your audience. I think when people hear the words patient engagement they think ‘Oh I’ve got to do something that will work for everybody,’ right? But like P.T. Barnum said, ‘you can’t please people all the time.’ I think patient engagement is a lot like that, I think it’s going to be customized, right? That’s why we have an EMR system that tracks all sorts of things about patients, like conditions and their demographics, and even whether they prefer phone or text messages for reminders and that type of thing. When you look at those types of campaigns, you almost got to think ‘Who are the people that are most likely to be engaged, and most likely to be engaged by this particular topic? All the push about Chronic Care Management, which is something CMS is reimbursing for now, and really targeting those things, and even saying those chronic care patients, those patients with those long-term, uncontrollable diabetes, those are the people who are more likely to respond so some sort of patient engagement and outreach.
John: Yeah, a couple things there, one is going back a little. A lot of doctors are afraid that if they start engaging patients, that they’ll reduce the number of office visits they get, and I’ve found the opposite to be true. Often, when they ask the question, for example, ‘Should I come in for an office visit?’ Then you end up driving more office visits and better office visits, because many of those people that are asking these questions and engaging with the doctor are ones that their choice is ‘OK, well I can engage online then I’ll do it, but if I can’t engage online then maybe I’ll skip the doctor completely.’ So then it just allows things to get worse — I think that’s one issue, too, that needs to be addressed and understand is that by engaging them, you can actually drive your fee-for-service visits, as well, because you’ll often engage people who would have just delayed that office visit until later. So I think that’s one side of things. But once you start engaging them, I think the other key, like you said, is the personalization and understanding, and many times that doesn’t have to be the doctor, that could be the nurse, it could be the front desk staff that could ask them the questions, that could engage them in a way, and then escalate it to an office visit, a telemedicine visit, or other things. But the real problem I’ve seen in most of the people’s implementation of this, is they do from a very tech-oriented standpoint. A great example is one that I think we’re going to talk about is this text message reminder service. It’s like — OK, well we want to make sure they’re compliant with their medication, right? That’s a great patient engagement solution, and we want to customize it, we know – OK, they should be taking this medication, and they haven’t filled it, so let’s just send them a text reminder to fill it. And you’re like, that’s great. WOuldn’ you want that, right? Because then you’re like, “OK, I forget to fill it, and I’ll do it.” Sounds reasonable, and it works for the 10% of people that aren’t taking their drug because they forgot, and that 10%, obviously, is flexible, but it’s a smaller percentage than we think. The reason that they’ve non-compliant to their medication is because they forgot. If the problem is that they forgot, then a text message works well. The problem is what about the other 90% of people, or whatever the specific figure is, whatever the other people aren’t taking it because they couldn’t afford it? Or aren’t taking it because they couldn’t get to the pharmacy? Or aren’t taking it because they don’t trust the doctor, and so they didn’t want to take because they don’t think the medication is actually going to fix the problem? So there’s this whole suite of other problems that exist, that we need to incorporate into our engagement efforts. Otherwise it’s just falling on deaf ears. Sure, it’s great that we help that 10% that actually benefitted because they needed a reminder, but if we do so, we can actually damage the other 90% by engaging with them in a way that actually shames them and makes them feel bad that they can’t take their drug because they can’t afford it, or whatever other problem there is.
Adam: So I think that goes back to making sure that that relationship, which is really what we’re talking about, we’re talking about ways that we can strengthen that relationship. I know I talked about PCMH briefly before, it really puts an emphasis on making sure when you prescribe a medication, asking the patient: “Are there any things that would make this hard for you to get? Do you have trouble getting to the pharmacy? Do you have trouble paying for your medication?” So that the practice can then try to incorporate some of that into the ways that it targets their patients, and sends the reminders to the appropriate people. So, theoretically, I think eClinicalWorks can do this. You can take that information that you’ve gathered, that you’ve put in your patient’s demographics or you’ve put into your patient’s chart and says ‘All right, we’d like to send out a medication reminder to all these people, but maybe we need to exclude, or send a different message to those people who’ve said they’ve had barriers, like financial barriers, or different types of things, so I think, really, that’s the power of the EMR. That’s kind of one of the reasons why we’re trying to make this push, is so that we can use this information in a more intelligent manner to guide this type of engagement and make sure patients feel more understood and more connected to their doctor.
John: But let’s not address it that way – what’s the real problem? Getting to the root problem and addressing it in a way that helps them actually change behaviors. So, for example, maybe you meeting someone and they’re not taking their drugs, or maybe they can’t get to an office appointment, right? So the tech solution would be like ‘Oh, we’ll send them an Uber credit,’ now they can get an Uber and go.. I’m a tech guy by background, that’s what we say ‘I just solved the problem.’ Well, was that the real problem? It’s like – well, is that the real problem? Well, if you look into it more, the real problem was was that they weren’t sleeping at night. And because they weren’t sleeping at night, they were depressed and because they were depressed, they lost their job, and because they lost their job they couldn’t afford their car payments, and now they don’t have a car and now that’s why they can’t get in there to do their appointment. So you really need to address the sleeping issue, not the car problem by sending an Uber, otherwise you didn’t really improve the care and you really didn’t understand the patient. So, I think you’re right, I think there’s multiple elements to this. One, you have to identify: What’s the real problem for the patient and then: What’s the right way to engage them? And that’s more behavioral science than technology.
Adam: Yeah, that’s a great point. That brings to mind of motivational interviews – I know my doctor does some of that figuring out. Do I know what I want out of my treatment, do I know what’s actually going to make me go through with it and follow through with it and that kind of stuff, knowing more about me. And that kind of leads me to the question of what do we think are some of the long-term effects we’re going to see in terms of reducing spending? Does patient engagement have the ability to move the needle? What do you think about that?
John: Well, I think it’s early to say for sure, but there’s great examples. I was thinking, when you told your story, I heard about this senior example, where they called them every day, or every week, or something like that, so they called them on a regular scheduled basis to ensure how is the senior doing? Are they following their compliance plan? And what was interesting from the study was they weren’t able to tease out, did it benefit the patient? Because they saw huge benefits to that patient population in lower costs, improved compliance, all of those things, but what we weren’t sure was – did the patient benefit because of the things we said on the call or because they knew a call was coming? And in the senior population, that’s a big deal, right? They’re the most expensive part of healthcare because they have so many chronic conditions, etc. But just the fact that they knew someone would call gave them something to look forward to, gave them something interesting, something exciting to change their day. They weren’t sure, they were still doing the research, and they’re like ‘OK, was it just the fact that we were going to call and engage them, once a day or once a week or whatever it was, or was it what we actually said on the call that really influenced the behavior change?’ So I mean it’s early days to really know what are the impact of some of these efforts, but I think there’s huge potential, we know that if we focus on these, I think we can put that improvement there. If we put more attention to it. The problem in the past is we didn’t pay anyone to do that. No doctor was paid to lower the cost of their patient’s care, in fact in many ways they were paid more to have more care. I mean, that was the business model. So it’s still early on in predicting how this will lower costs and will this do it effectively, but I think there’s huge promise if we do it the right way. Another example that’s interesting really comes from C.T. Lynn that we talked about previously. He’s done a lot of work on when should you give the lab results or the xray results or the other various results in the patient portal because that’s another way to engage them because if you give them the result early they don’t stress as much. If it’s a normal result, just push it out, don’t wait for the doctor to read it. They’ve seen an interesting revolution though — how quickly can they get them out? What they’ve found is that for a lot of results, you may want to have a two-to-three-day wait, because if you’re going to tell them ‘You have cancer’ or you’re going to tell them ‘Your baby is dead because of some lab tests that realize oh your baby’s dead and we’re going to have to do a DNC and take your baby out.’ You know, these really life-changing types of results, you need to give a certain period of time to be able to do that. But I heard him talk recently and they had an experience that forever they’ve given out the result immediately, in real-time fashion, to all of these mothers about their child, and then they looked at it and they had this really bad incident where someone got it on a Friday evening and then they had it all weekend, stressing, and they weren’t hearing back from the doctor and there’s all this chaos – ‘Oh we should never give it, now that we know it’s a good result.’ He’s like ‘OK, let’s relax, we’ve pushed out these result for three years,’ or whatever it was, like a long period of time, two or three years, and no one has had any issue with it – in fact, patients love it because then they know early, and they don’t have to wait for the doctor to read it and do it. He’s like ‘So, are we just overreacting over this one incident, when we’ve had it for years that proves that it’s really not as big of an issue as it is.’ So I think there’s going to be some evolution as people learn when is the right time to do it, and how do we present it, and I think we’re going to see a huge evolution in that. In fact, I think eCW will play a big role in that as when you provide lab results, when you provide them diagnoses, when you provide them CPT codes or plans, how is that going to be ingested by the patient? Is it going to be done in a way that they understand it, they can process it, that they can understand what’s normal, that they can understand when it’s OK for it to be abnormal and that they shouldn’t stress about it because they have higher levels because of this other disease. I mean, that’s going to become really sophisticated and we’re really going to help with health literacy with the patient, so that they really understand what the results mean and that’s going to happen electronically, that’s not going to happen through people. So I think maybe that’s the next level of engagement — is really facilitating those types of things, and whether it comes through the portal, a text message, whatever other means that you communicate to the patient, we’re going to have to work hard on making it so that the patient can understand what that data means.
Adam: Yeah, good point and, like you said, maybe one of the things is to set up a rule so that your lab results that are getting published don’t go out after 2 PM on a Friday or something like that. That’s certainly possible. In eClinicalWorks, I know that for certain tests or when you review the lab, the lab result doesn’t go to the patient portal until it is reviewed. So, for those extra sensitive things, you can say ‘Hold this back,’ and then the rest of them will go, the rest of them will go to the portal. So there are those capabilities, but, as you said, it’s going to get more sophisticated, more refined, more tailored, as we learn more and gain that experience. But I think the other really important thing that you mentioned there is they did this for three years, and had one really serious, bad incident. We’ve talked about fear before, doctors are afraid this is going to negatively impact them, but I think that one incident over however many thousands and thousands of labs that must have been sent out, it’s a very small occurrence. I think it’s reasonable to expect one or two situations like that, and I think the ultimate takeaway is that don’t be afraid to put this in place. The benefits seem to outweigh the risks there. So for a final question, John, who really needs to take responsibility for patient engagement? Is it the doctors, is it the vendors, is it the patient? You have on your website, a conversation you had with some people from the L.A. health quality forum, who had great success with patient engagement and a campaign that they did state why there. So who’s going to help make this a success?
John: So, yeah, the Louisiana health quality forum is really interesting, because they are literally actually doing the marketing effort to get patients engaged in Louisiana in their care and to get them signed up on portal, to get them to participate in portals — that’s a unique effort. But I think we can learn a lot from them because what they’ve found is you’d be surprised by who wants to access that. They have stories of these old men who want access to their patient portal. They barely use technology and yet they want to be there on the portal getting access to their healthcare and getting access to their information. So I think that’s the first step and I think that we need to be careful who we judge might be interested in engaging with doctors and their care. The answer is we all have to, we all play a role. If the technology solutions aren’t there to engage the patients, then doctors won’t do it. If doctors don’t want to engage the patient, they’re not going to. Although there’s some incentives trying to push that direction and helping afford that. And if a patient doesn’t care, the doctor can try to engage the patient all together they want, but if they don’t illustrate to the patient why it’s worthwhile for them to engage with the doctor, it’s not going to happen. So it really takes everyone involved, and it takes the right approach that actually adds value, as opposed to these kind of topline things that don’t really change the care and don’t really engage the patient — they don’t improve care, they don’t make it easier for anyone. That’s the problem. But as we focus on more efforts that really do improve our care, and we can quantify the way a patient’s impacted, that’s where we’re going to really see huge increases in engagement from patients.
Adam: And you mentioned there’s a learning curve there is what it sounds like you’re mentioning there’s a right way to do the patient engagement, and just to let people who are watching know – eClinicalWorks, we have lots of case studies that you can learn from on our website, we have lots of videos and other conversations on our other podcasts with people who’ve been there, who’ve done that. You can learn from their experiences. So, definitely check those things out for those of you who are watching.
John: I was at a conference recently, I think it was Amy Cuddy that said ‘We need more people in healthcare to care.’ I think that describes it best.
Adam: Good words, yes, absolutely pertinent and definitely words to live by. Well, John, thank you so much for taking the time to speak with us today, it’s been a great conversation, hopefully we can do it again in the future, and for those of you who are watching, check out healthcarescene.com — they’ve got lots of different blog threads you can follow on all aspects of healthcare and some great videos and conversations and articles to read there, as well. So John, thanks for your time, and we’ll talk to you soon. Thank you.
Adam: Thanks for watching the conclusion of our interview with John Lynn from healthcarescene.com. Now, if you missed it, you can also find part one on YouTube, iTunes or my.eclinicalworks.com, and if you’d like to see more episodes, you can check them out there, as well. For the eClinicalWorks podcast, I’m Adam Siladi, and thanks for watching.

