eClinicalWorks® (eCW) provides enterprise healthcare solutions to improve and streamline the operations of your multi-provider organization (MPN) with scalable solutions and technologies that consolidate your data and centralize your billing. From seamless onboarding to unified support and optional Revenue Cycle Management (RCM) services for clinics at just 2.9% of collected revenue, we’ve got you covered to promote your growth and help you save.
We recognize that MPNs come in many forms. The right enterprise-based solutions are essential for ensuring smooth cooperation among networks, optimizing data sharing, and enhancing the quality and efficiency of care.
Flexible, Scalable Infrastructure Solutions
Leverage AI to Optimize Your EMR Efficiency
We help you grow and succeed with an AI-powered EHR for more efficient operation of your entire organization — including the front office, the back office, and clinical care.
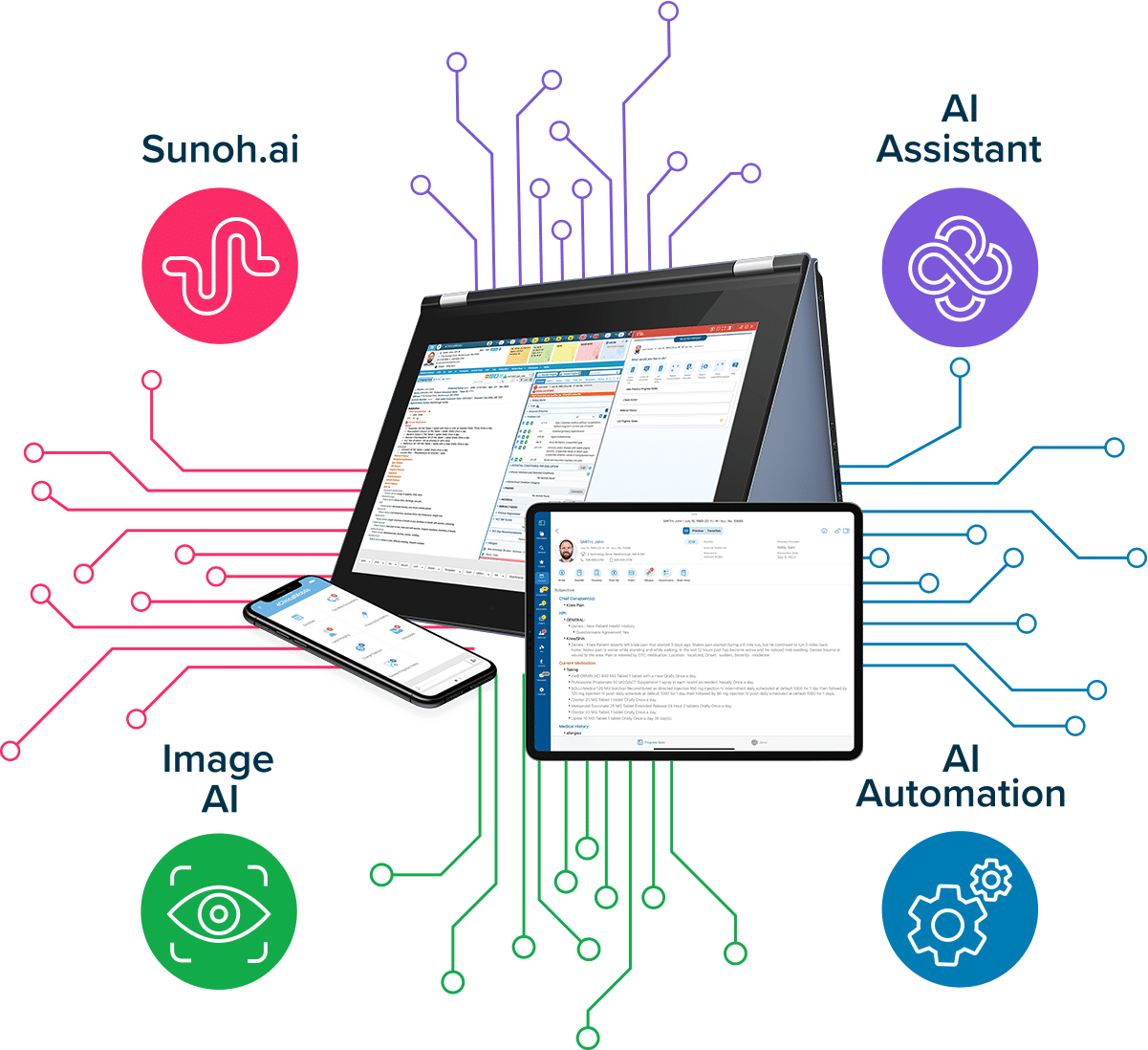
Leverage AI to Optimize Your EMR Efficiency
We help you grow and succeed with an AI-powered EHR for more efficient operation of your entire organization — including the front office, the back office, and clinical care.
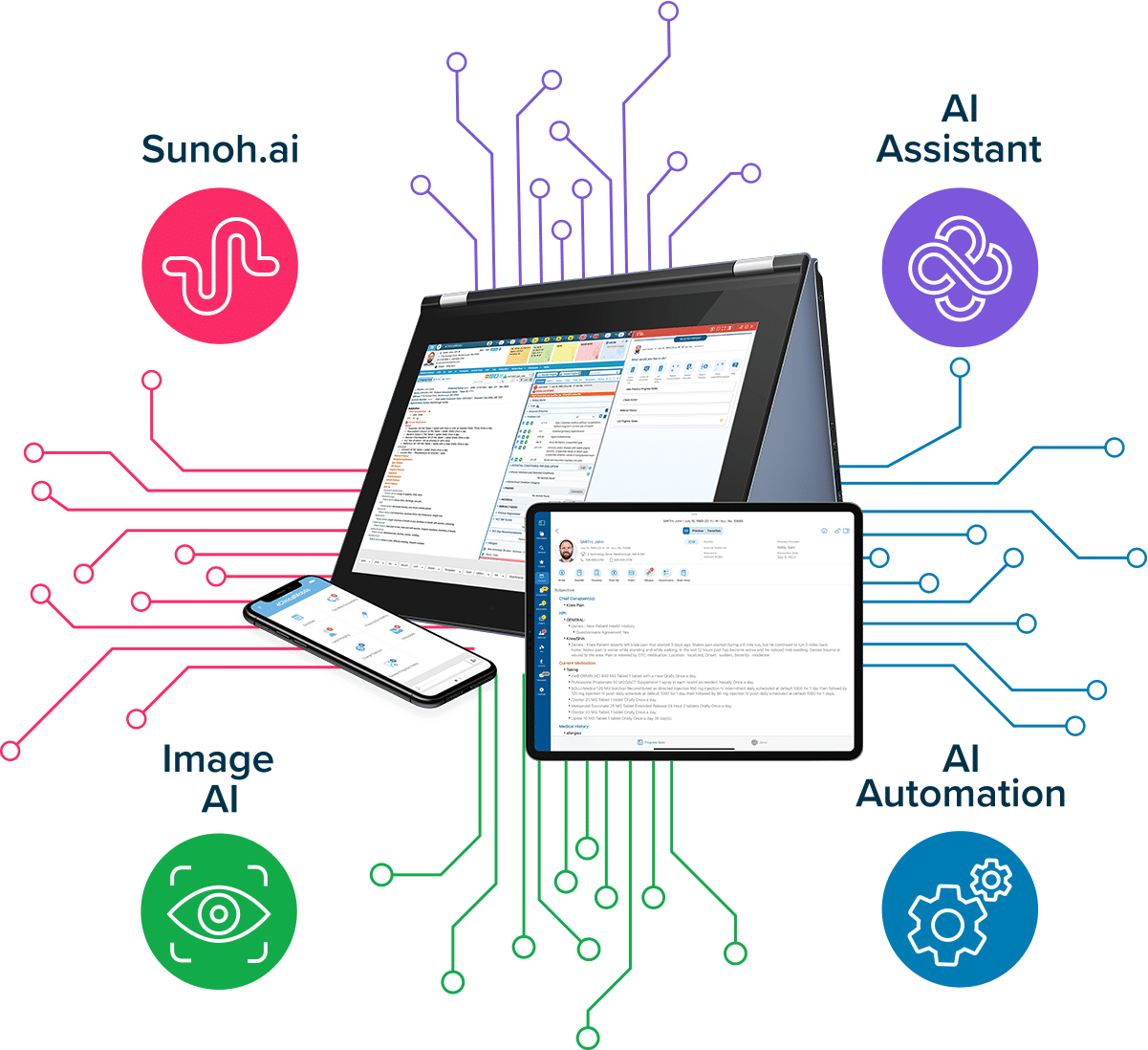
AI for Revenue Cycle Management
- Streamlines the Revenue Cycle Management billing process, replacing RCM as a service with automated, intelligent workflows.
- Includes AI-powered insurance eligibility response and EOB-to-ERA conversion, which enhance efficiency across front- and back-office operations.
- Automates the appeals process by generating appeal letters and speeding up denials management while improving accuracy.
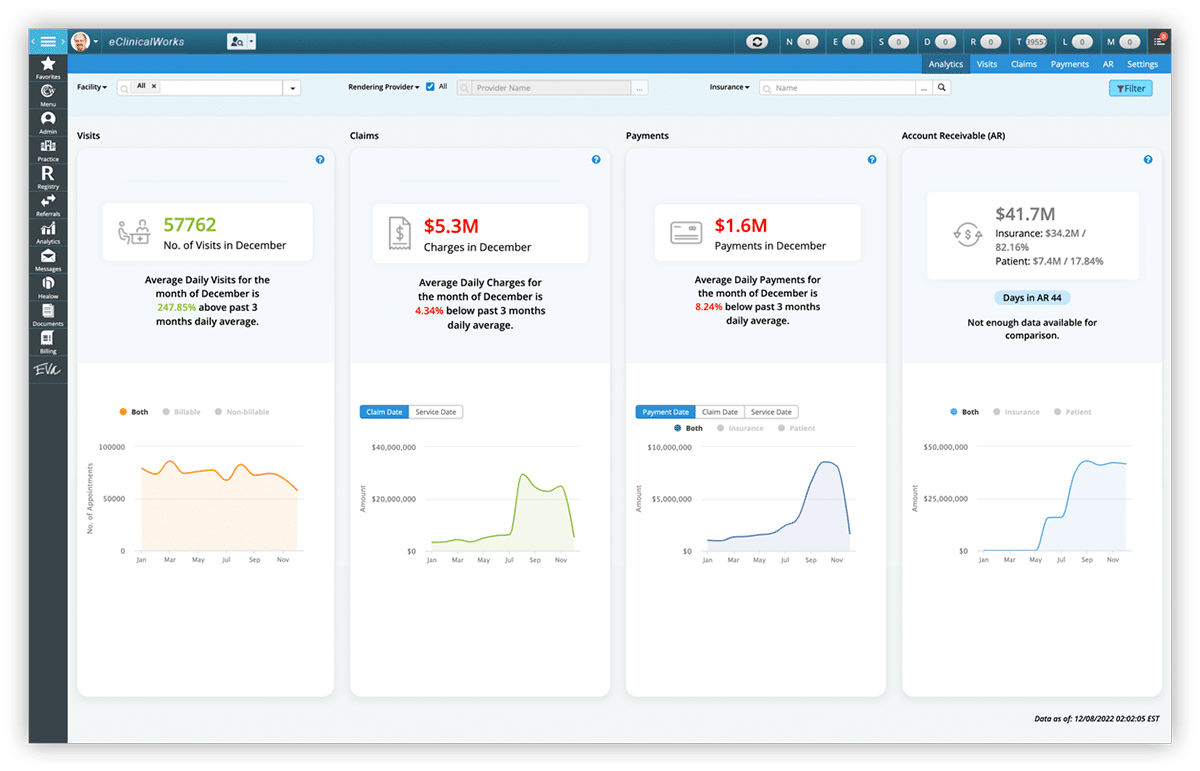
- Provides quick access to claims, collections, denial management, and payments via a deep search function. At the same time, AI-powered analytics enable interactive dashboards and natural language interactions, offering actionable insights for improved financial outcomes.
AI for Revenue Cycle Management
- Streamlines the Revenue Cycle Management billing process, replacing RCM as a service with automated, intelligent workflows.
- Includes AI-powered insurance eligibility response and EOB-to-ERA conversion, which enhance efficiency across front- and back-office operations.
- Automates the appeals process by generating appeal letters and speeding up denials management while improving accuracy.
- Provides quick access to claims, collections, denial management, and payments via a deep search function. At the same time, AI-powered analytics enable interactive dashboards and natural language interactions, offering actionable insights for improved financial outcomes.
Simplify Data Management and Improve Decision Making
We provide you with the powerful tools you need to make data management easy and to make smarter decisions across your entire healthcare ecosystem.

PRISMA
Aggregate patient data from multiple sources into a searchable health record for a more complete patient view.
Nationwide Interoperability Networks
Enjoy seamless exchange of data across your network, including patient records from other facilities on shared interoperability networks.
FHIR Integration
Access and share healthcare data with other systems through Fast Healthcare Interoperability Resources.
Interoperability
Gain and maintain connections with hospitals, labs, and other networks.
