The First Step: Patient-Centered Medical Home
- 17 March 2022
- Blog
eClinicalWorks
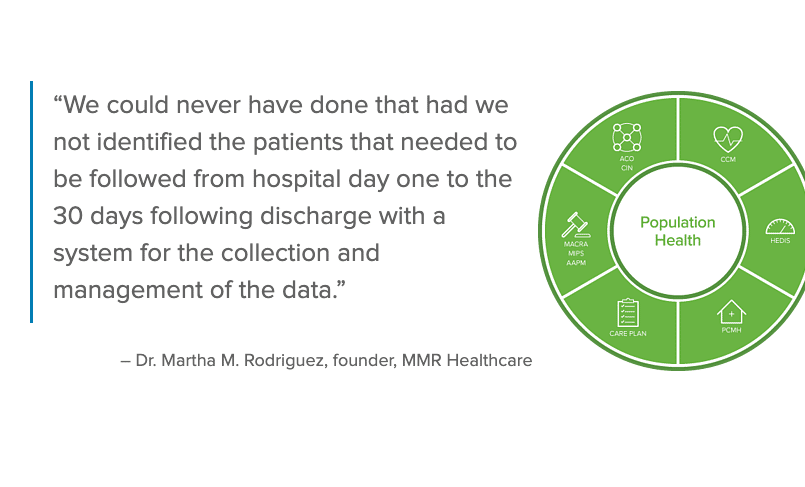
To get started with Population Health, there’s no place like PCMH
Just as no building can long endure without a strong foundation, medical practices that hope to grow and thrive in an age of value-based healthcare need to build upon fundamentals.
Once viewed as something that could be grasped and practiced only by the most advanced medical practices, Population Health Management (PHM) is now widely recognized as one of those fundamentals and a key means of delivering quality care.
Patient-Centered Medical Home can be the key to unlocking the mysteries of PHM.
The country doctor in times gone by may have had complete knowledge of every patient — and perhaps even several generations of the same family — but that is simply no longer the case.
Today’s medical providers typically treat thousands of patients. The scale and complexity of healthcare mean that, if providers are to succeed, they must devise ways to be more efficient in the delivery of care. That means recognizing patterns and harnessing tools that can address common needs across an entire panel of patients.
In short, they need Population Health Management.
With the right tools, PHM is achievable by any practice
Even something as simple as identifying which patients are overdue for a colonoscopy qualifies as a PHM task — and can be laborious and time-consuming without the right tools. Other PRM activities, such as managing patients with multiple chronic conditions and keeping track of which patients are being hospitalized and why, can quickly become daunting — again, if a practice is trying to achieve those goals without a strong healthcare IT partner.
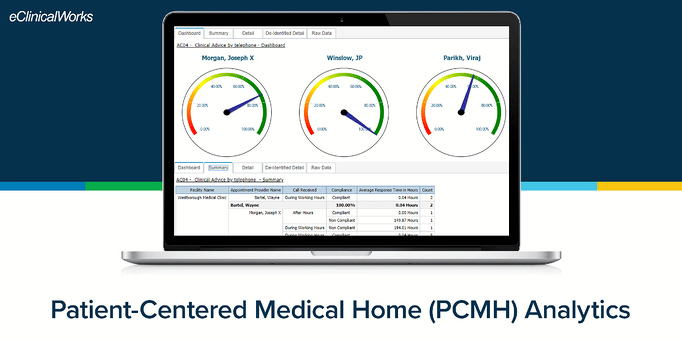
In fact, eClinicalWorks® and healow® offer practices of all types and sizes a wealth of solutions for PHM activities. We’ll be exploring many of those solutions in depth in coming installations of this blog series.
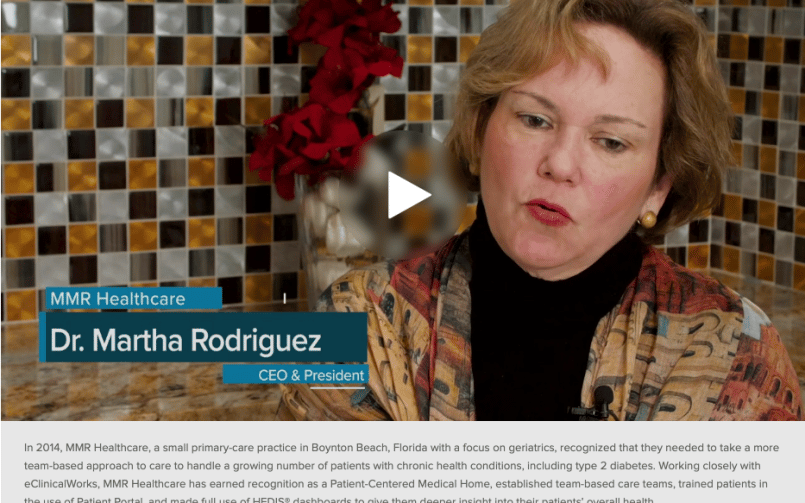
But we focus first on Patient-Centered Medical Home Watch the short video below to see how eClinicalWorks helps practices achieve PCMH recognition.
Why do so many practices focus on PCMH? Because achieving recognition means that a practice has the right architecture upon which to build a more efficient operation, with clearer lines of communication and stronger relationships with both patients and other medical organizations. It sets the stage for success in every other aspect of PHM.
What exactly is PCMH, and why does it matter?
According to the National Committee for Quality Assurance (NCQA), PCMH is a self-guided operational excellence program that puts patients at the forefront of care by fostering stronger relationships between patients and their clinical care teams.
More than 10,000 practices — encompassing some 50,000 clinicians nationwide — have achieved PCMH recognition.
According to a 2018 Milliman white paper prepared for the NCQA, practices that seek PCMH recognition focus on standards and guidelines in six key areas. They may:
- Improve relationships with specialty care physicians
- Build greater awareness of and increase referrals to community-based resources
- Enhance the reputation of their practice
- See improvements in patients’ adherence to care plans
- Bolster PHM and improvement efforts
- Reduce medical liability insurance
Evidence shows PCMH is effective
The Millman paper explores both the operational and revenue advantages that can result from achieving PCMH recognition.
- Whereas most practices lose between 3% and 14% of revenue to no-shows and cancellations, PCMH practices can minimize these losses and may see overall increases in practice revenue.
- Practices with PCMH recognition can save money by reducing hospital and ER visits and improving patient outcomes.
- Many of the prerequisites for PCMH recognition overlap with requirements for other value-based payment models, meaning that practices are in a better position to take advantage of additional financial incentives.
To learn more about how eClinicalWorks can help your practice get started with the PCMH recognition process, contactpophealthsales@eclinicalworks.com
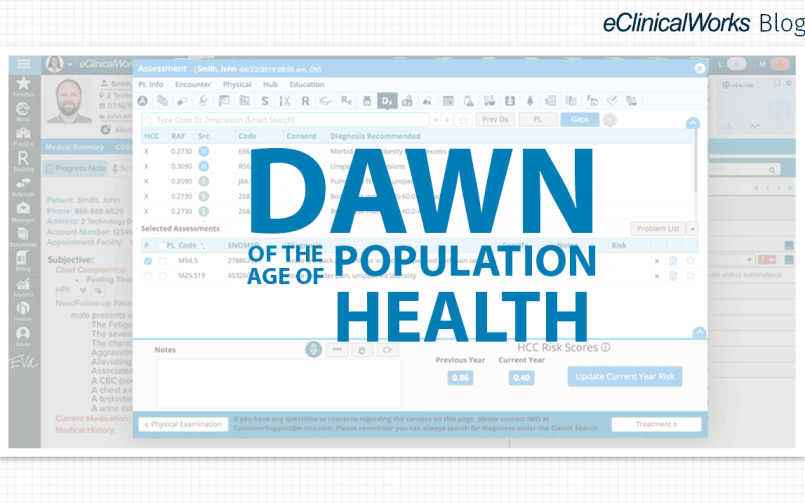
Next month, our Population Health blog series looks at Hierarchical Condition Category (HCC) coding and how eClinicalWorks helps practices engaged in value-based reimbursement more accurately measure their patient populations, calculating risk acuity to predict expenditures.