The Cornerstone of Value-Based Care: 4 Facts About Annual Wellness Visits
- 3 January 2025
- Blog
Aledade
This blog is presented by Aledade as part of their sponsorship of the 2024 eClinicalWorks® and healow® National Conference.
In today’s rapidly evolving health care landscape, the focus is shifting from reactive treatment to proactive and preventive care. This transformation is particularly pivotal for Medicare beneficiaries, who often require comprehensive management of their health to prevent the escalation of chronic conditions. At the heart of this shift is the Annual Wellness Visit (AWV), a cornerstone of high-quality primary care that not only fosters a healthier patient population but also supports the financial sustainability of health care providers.
1. Transitioning the Patient-Doctor Relationship from Reactive to Proactive
The traditional patient-doctor relationship has long been characterized by a reactive nature, where patients present with symptoms, and physicians respond accordingly. However, the AWV changes this dynamic by prioritizing preventive care and long-term health planning. During these visits, the conversation extends beyond immediate health concerns to encompass a holistic view of the patient’s well-being.
For instance, a typical office visit may focus on addressing a patient’s chronic back pain, whereas an AWV allows for a more comprehensive discussion about lifestyle factors, future health goals, and preventive measures. This proactive approach encourages patients to engage in their health management actively, ultimately leading to improved health outcomes. Studies have shown that when patients participate in regular AWVs, they are more likely to receive recommended preventive services, such as screenings and vaccinations, which can thwart the progression of potential health issues.
This shift also presents challenges, such as encouraging patients to adopt lifestyle changes discussed during the AWV. To mitigate this, health care providers can utilize motivational interviewing techniques, which help patients articulate their health goals and barriers, fostering a more meaningful commitment to change.
2. Enhanced Health Outcomes and Reduced Costs of Care
The strategic design of AWVs not only improves individual health outcomes but also contributes to cost savings for both patients and health care systems. By identifying potential health risks early on, AWVs help in reducing the need for more expensive and invasive treatments later. Medicare beneficiaries benefit from these visits as they are fully covered without out-of-pocket expenses, making them accessible and encouraging consistent attendance.
Moreover, health care providers are incentivized through enhanced reimbursement rates, often up to 50 percent higher than standard evaluation and management visits. This financial model supports primary care organizations in achieving shared savings. For example, a primary care clinic that consistently conducts AWVs may notice a decrease in emergency room visits and hospitalizations among its patient population, thereby lowering overall health care costs and enhancing the clinic’s financial stability through shared savings programs.
However, the implementation of AWVs requires careful consideration of resource allocation and staff training. Health care providers must balance the increased demand for these services with the existing workload, ensuring that AWVs do not compromise the quality of care delivered during other visits.
3. The Importance of a Team-Based Approach
The successful implementation of AWVs within a primary care setting hinges on a collaborative, team-based approach. While physicians play a key role, they are not the sole participants in conducting AWVs. Physician assistants, nurse practitioners, and other licensed medical professionals can also lead these visits, broadening the scope and efficiency of care delivery.
Pre-visit planning is a pivotal component of this team-based strategy. Support staff, for instance, are responsible for preparing detailed patient information, performing initial health assessments, and conducting necessary screenings. This preparatory work ensures that the physician has comprehensive data at their fingertips, allowing for an informed and efficient AWV.
An illustrative example of this approach can be seen in a community health center where a registered dietitian collaborates with the primary care team to address nutritional concerns during the AWV. Such interdisciplinary collaboration enriches the visit’s content and provides patients with a more rounded perspective on their health.
Additionally, the integration of technology, such as electronic health records (EHRs), enhances the efficiency of AWVs. EHRs facilitate seamless communication among team members, ensuring that all relevant patient information is readily accessible and up to date. This technological support not only streamlines the AWV process but also improves patient engagement by allowing them to view and understand their health data more easily.
4. Accurate Documentation: The Backbone of Value-Based Care
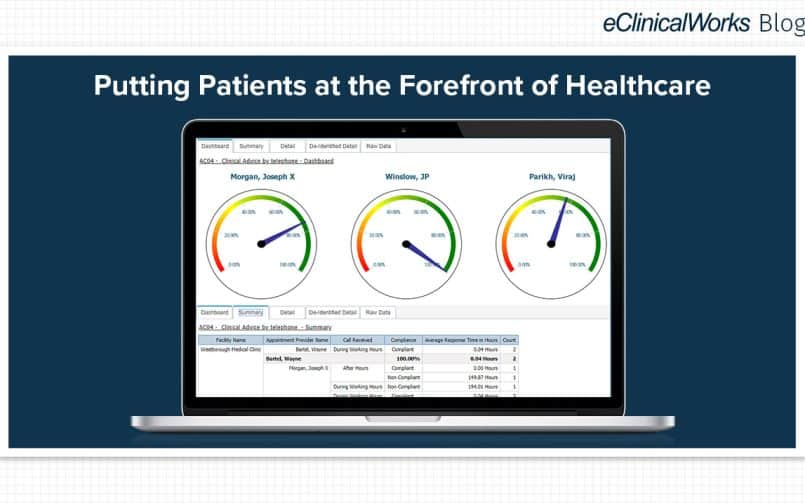
In value-based care models, accurate and complete diagnosis documentation is essential for aligning with spending benchmarks and unlocking shared savings opportunities. The clinical complexity of a patient population significantly influences these benchmarks, and AWVs provide an opportune moment for thorough documentation.
Utilizing electronic health records (EHR) with structured templates can streamline this process, ensuring that every aspect of patient care is recorded and credited appropriately. This not only enhances the accuracy of patient records but also aids in closing quality measure gaps. For instance, a physician might use an EHR template to document a patient’s progress in managing diabetes, capturing improvements in lifestyle and medication adherence that are crucial for measuring care quality.
Through precise documentation, health care providers can demonstrate the value of their care and substantiate the preventative measures taken during AWVs. This, in turn, reinforces the financial viability of value-based care models and ensures that providers are rewarded for delivering high-quality, proactive care.
However, the transition to digital documentation can pose challenges, including the need for staff training and the potential for technical issues. To address these, health care organizations can invest in ongoing training and support to ensure that all team members are proficient in using EHR systems effectively.
Conclusion
Annual Wellness Visits represent a pivotal shift in how Medicare beneficiaries receive care, emphasizing proactive management and preventive strategies. By fostering a strong patient-doctor relationship, improving health outcomes, and engaging a team-based approach, AWVs play a critical role in the evolution of primary care. Furthermore, the emphasis on accurate documentation not only aligns with the goals of value-based care but also ensures the sustenance of health care practices.
As the health care landscape continues to evolve, the prominence of AWVs will only grow, serving as a vital tool in achieving healthier populations and more efficient health care systems. For Medicare beneficiaries and providers alike, embracing the benefits of AWVs is a step towards a more sustainable and health-focused future. The integration of technology and team-based care will further enhance the effectiveness of AWVs, ensuring that patients receive the comprehensive, proactive care they deserve. To learn more about value-based care, visit our resources page.