Solutions for the top five credentialing challenges
- 5 December 2024
- Blog
TriZetto Provider Solutions
This blog is presented by TriZetto Provider Solutions as part of their sponsorship of the 2024 eClinicalWorks® and healow® National Conference.
Credentialing is a critical process for healthcare organizations of all sizes. They ensure providers are qualified and authorized to deliver care. Despite its importance, credentialing comes with a set of challenges.
Here are the top five obstacles organizations encounter with credentialing and some strategies to address them.
1. Managing timelines and deadlines
Credentialing is time sensitive and directly impacts payments and reimbursements. Delays can lead to credentialing-related denials and significant financial losses.
Challenges:
- Initial credentialing: Aligning the onboarding process with credentialing timelines to ensure providers can see patients as soon as they’re ready can be difficult.
- Re-credentialing: Missing deadlines, which can be caused in part by the lack of a dedicated credentialing specialist, can result in providers being out of network for 90 to 120 days.
- Payer turnaround times: Navigating the varying timelines of multiple payers which have been impacted by industry challenges like technology gaps and staffing issues, can be arduous
Solutions:
- Implement a robust onboarding process that has appropriate tracking mechanisms.
- Automate reminders and follow-ups to ensure timely submissions for re-credentialing.
- Set clear expectations with providers to promptly gather necessary information.
- Have a clear understanding of the timelines of the plans you are credentialing.
2. Finding and retaining experienced credentialing staff
Experienced staff are crucial for efficient and accurate credentialing. Provider organizations that lack knowledgeable credentialing professionals run the risk of missing credentialing deadlines, losing revenue and becoming non-compliant with their licensing.
Challenges:
- Competitive job market: It’s often difficult to find and retain knowledgeable credentialing staff.
- Budget constraints: Rising costs and limited budgets make it challenging to scale credentialing teams as needed.
- Staff turnover: High attrition rates can disrupt the credentialing process and lead to inconsistencies.
Solutions:
- Offer competitive salaries and benefits to attract and retain skilled staff.
- Provide ongoing training and professional development opportunities.
- Utilize technology to streamline processes and reduce the manual burden on staff.
3. Data management
Effective data management is essential for maintaining accurate and up-to-date credentialing records. Failure to do so can create a lack of credibility and lead to revenue loss.
Challenges:
- Volume of data: Managing large volumes of data, including sensitive information like social security numbers and banking details, is time-consuming and takes significant resources.
- Manual processes: Many organizations still rely on manual processes, leading to inefficiencies and errors.
- Data security: Securing sensitive information is paramount, especially in light of increasing cybersecurity threats.
Solutions:
- Implement electronic data management systems to centralize and secure credentialing information.
- Automate data collection and validation processes to reduce manual errors.
- Regularly update security protocols to protect sensitive information.
4. Privacy and security
Protecting the privacy and security of provider information is critical to maintaining trust and compliance with regulations. Without a HIPAA compliant platform, provider organizations expose themselves to potential data breaches and other legal issues.
Challenges:
- Sensitive information: Credentialing involves collecting and storing sensitive information like patient health information (PHI) which must be protected from unauthorized access.
- Data transmission: Securely transmitting data between providers and credentialing teams can be challenging without a secure, HIPAA compliant data management system.
- Cybersecurity threats: The healthcare industry is a prime target for cyberattacks because of the value of private patient and provider information, making robust security measures essential.
Solutions:
- Use secure, cloud-based systems for storing and accessing credentialing data.
- Implement strong encryption and access controls to protect data during transmission.
- Conduct regular security audits and training to stay ahead of potential threats.
5. Manual processes
Reducing manual processes can significantly improve efficiency and accuracy in credentialing.
Challenges:
- Application submission: Manual data entry for credentialing applications is time-consuming and prone to errors.
- Re-credentialing monitoring: Manual tracking of re-credentialing timelines can lead to missed deadlines and revenue loss.
- Task management: Managing tasks manually can result in delays and miscommunication.
Solutions:
- Automate application submissions using bots to ensure accuracy and speed.
- Implement automated systems for monitoring re-credentialing timelines and expiring information.
- Use task management software to streamline communication and follow-ups with providers.
By addressing these challenges with strategic solutions, healthcare organizations can improve their credentialing processes, reduce administrative burdens and ensure timely and accurate provider authorizations.
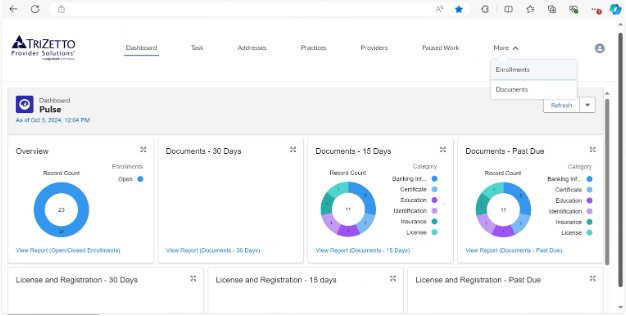
Credentialing from TriZetto Provider Solutions
Provider organizations can utilize TriZetto Provider Solutions’ intuitive credentialing portal coupled with expert-supported service to gain an end-to-end solution for their organization’s credentialing needs. The guided workflow helps organizations achieve compliance quickly, saving valuable time and allowing quicker reimbursements for services.
Learn how you can improve document management, eliminate data redundancies and ensure compliance with our credentialing service by visiting trizettoprovider.com/solutions/credentialing.