Show Me the Bots! (And the Money)
- 21 July 2022
- Blog
eClinicalWorks
How RPA in RCM can improve your bottom line
If you were on a walk and spotted a couple of billion dollars by the side of the road, odds are you would do something about it. But each year, healthcare organizations — hospitals, clinics, and practices — collectively lose billions of dollars to administrative costs, losses that could be avoided with more efficient Revenue Cycle Management (RCM) practices.
According to a 2020 report by the Council for Affordable Quality Healthcare, Inc. (CAQH), healthcare practices could have saved $16.3 billion in 2020 simply by switching from time-consuming, error-prone manual processes to automated ones.
“Shifting from manual tasks to an automated process workflow will reduce time spent per task from minutes to fractions of a second,” the Medical Group Management Association notes in an article assessing the CAQH report. “Case studies show that manually posting payments and denials takes 2.10 minutes per claim, compared to a rate of 2 seconds per claim with robotic process automation (RPA).”
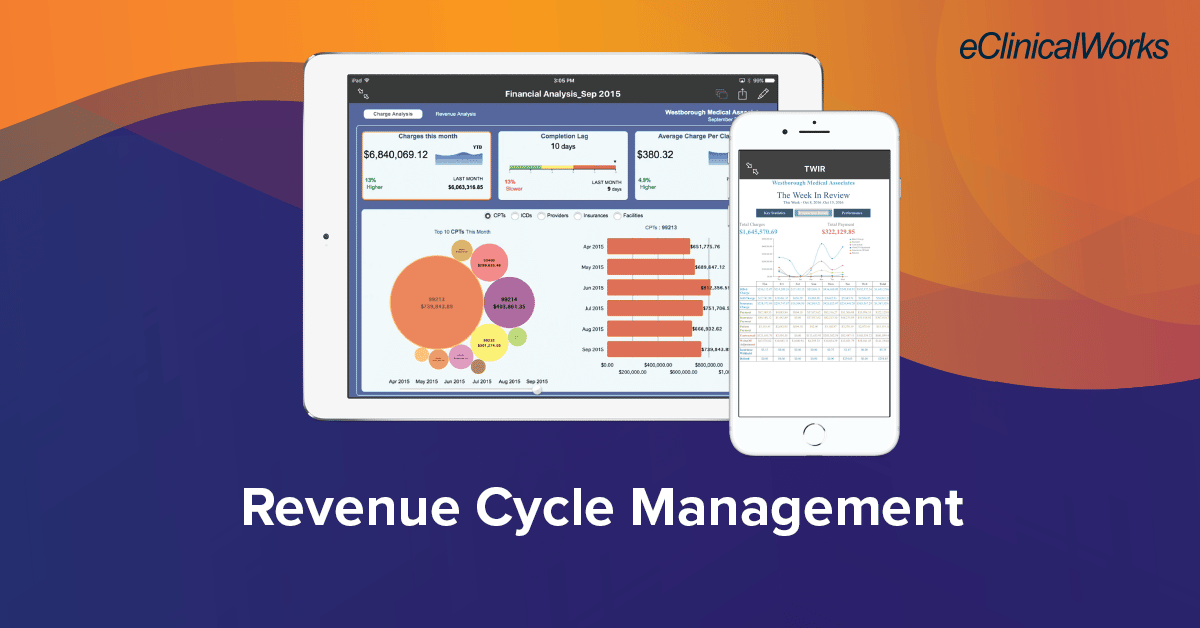
How eClinicalWorks is leading the way
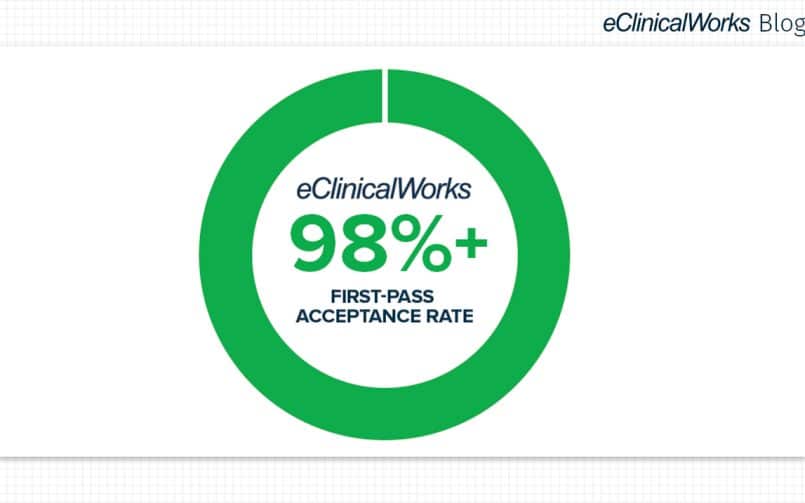
How can your organization put RPA to work to improve efficiency? By partnering with eClinicalWorks and choosing the RCM solution that works best for you. Whether you choose to do your own billing or use our end-to-end RCM billing service, our bots will be there to improve the efficiency of your operations.
That can mean faster collections, a 98.6%+ first-pass acceptance rate, lower days in accounts receivable (A/R), and a sharp reduction in the errors and delays that characterize many practices’ billing operations.
Meeting key RCM goals
One overarching goal for practices is to simplify their operations.
“Our goal was to remove multiple legacy software vendors and increase efficiency while reducing administrative burnout and costs for back-office staff,” said Derek Armstrong, CEO of Midwest Orthopaedic Center, a practice with nearly 50 providers serving Central Illinois. “eClinicalWorks’ technology meets that need perfectly.”
Another key target is reducing days in A/R.
“We’re at a 99%+ in net collections ratio for insurance claims,” said Todd Mallon, Chief Financial Officer at New Jersey-based Advocare, LLC. “The only thing I used to talk about was accounts receivable, and today, three years into this, the only thing I don’t talk about is accounts receivable!”
An industry shift toward automation
Overall, the healthcare industry is making progress toward automation in Revenue Cycle Management, but less quickly than one might expect.
One survey taken last August, for example, found that 78% of hospitals had already implemented or were implementing automation for their RCM, up from 66% just a year before. That means that nearly one in four hospitals is still far less efficient than it might be.
And the opportunities for improvement extend beyond hospitals. As the CAQH report notes:
“While the industry continues to make progress automating administrative tasks, opportunities remain. Although electronic transactions have become more efficient, transactions that continue to be processed through partially electronic web portals and manual methods are becoming more expensive and time consuming. To address these automation gaps, standards and operating rules need to be updated more frequently to adapt to changing business needs.”
Why wait to reclaim your money? Click here to learn how eClinicalWorks can revolutionize your practice’s RCM.