Revenue Cycle Management: Boosting Operational Efficiency and Productivity
- 20 September 2024
- Blog
eClinicalWorks

Efficient revenue cycle management is crucial for operational success. Health centers often face challenges in revenue management, handling a high volume of claims may lead to errors and rejections. Navigating complex billing processes and regulatory compliance can add to the burden, causing delays in payments. Additionally, limited staff can stretch the capacity for effective claims management, impacting the cash flow and overall financial health.
A robust RCM solution can streamline claim management for health centers by automating the billing process, reducing errors, and ensuring timely submissions. It improves claim accuracy, minimizing rejections and denials, and speeds up the revenue cycle. By freeing up staff from manual tasks, a right RCM solution allows them to focus on more strategic activities, enhancing both productivity and financial health.
Preventive Approach to Managing Claims
A preventive approach to managing claims involves proactive strategies to minimize errors and rejections before claims are submitted.
- This includes thorough patient data verification, accurate coding, and compliance checks with insurance requirements.
- Using advanced RCM tools to detect potential issues early also play a key role.
- By addressing problems upfront, health centers can improve claim acceptance rates and optimize revenue cycles.
Streamlining Operations
An RCM solution streamlines operations in a health center by automating routine tasks.
- It can enhance communication through real-time status updates and centralized dashboards, keeping teams informed and aligned.
- By providing tools for efficient collections and alerts, it ensures everyone is on the same page, improving both internal coordination and patient interactions.
Time Savings for Billers
Automating routine billing tasks, allows billers to concentrate on high-priority activities.
- By reducing manual data entry and minimizing errors, billers can focus on resolving complex claims and enhancing revenue cycle strategies.
- This shift allows them to support improved patient care by addressing financial issues swiftly, leading to faster claim resolutions and increased patient satisfaction.
- With more time for strategic tasks, billers can contribute to a smoother, more patient-centric healthcare experience.

Improving Practice Revenue
Reduced claims directly translate to increased revenue.
- An end-to-end RCM solution can enhance practice revenue by streamlining billing processes, reducing claim denials, and accelerating payment cycles.
- By automating tasks like coding and insurance verification, it minimizes errors and ensures faster reimbursements.
- This efficiency allows healthcare practices to focus more on patient care while optimizing their financial performance.
Ohio-based Knox Public Health struggled with rejected claims, outstanding claims, and unposted payments. Upon optimizing eClinicalWorks® RCM Service Model, the health center witnessed significant results:
- The integration of eClinicalWorks RCM dramatically reduced denial rates and backlog of unposted payments
- There was a substantial decrease in outstanding claims
- A new setup ensured the backlog of Medicaid claims is now being processed efficiently, and over 1,400 claims that were stuck in the system have already been submitted.
As a result, the practice was able to improve operational efficiency, automation of claim creation and submissions enhanced productivity and revenue.
eClinicalWorks® RCM Service Model offers an end-to-end solution for large health centers as well as small and independent healthcare practices. eClinicalWorks RCM experts utilize the billing technology to its full potential, taking a preventive approach to managing denials and rejections. They continually monitor and assess the health center’s financial health through real-time dashboards and on-demand reporting.
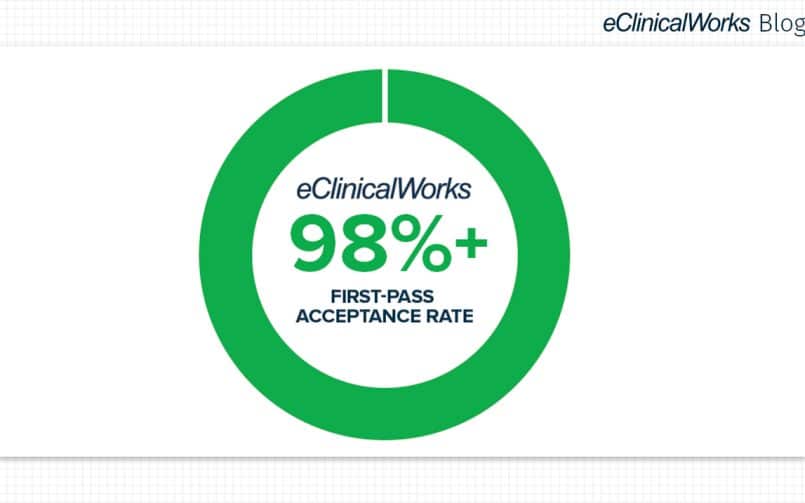
Partnering with eClinicalWorks industry-leading quality, RCM solutions allow healthcare practices to leverage outstanding customer support, live dashboards, on-demand reporting, and a 98% or higher first-pass acceptance rate. Click here to learn more.