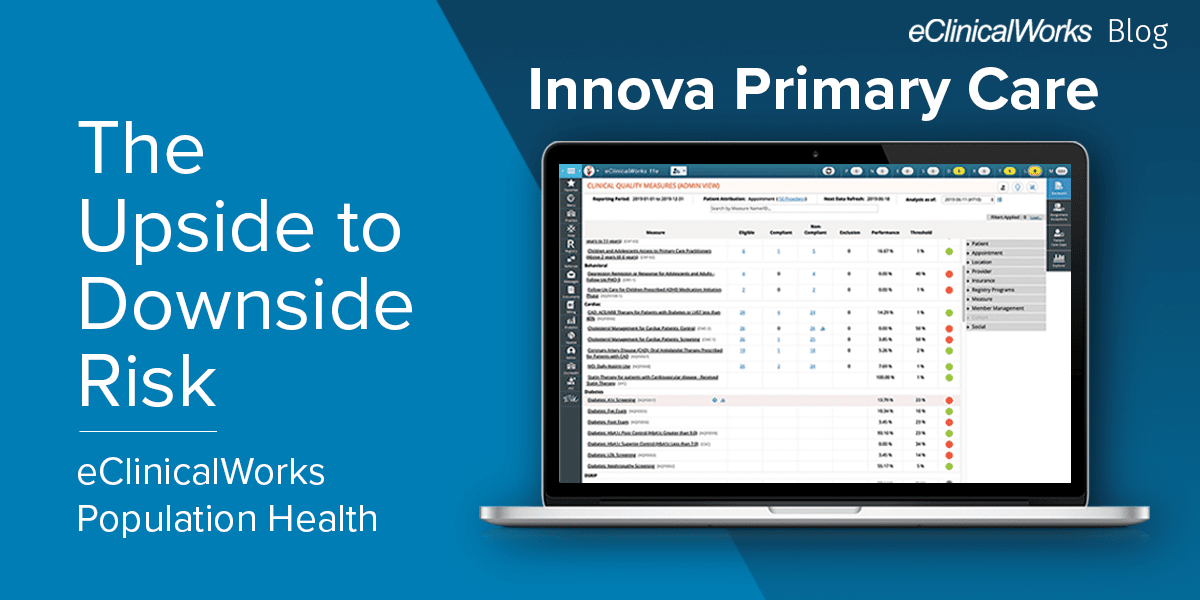
Innova Primary Care: The Upside to Downside Risk
- 2 November 2021
- Blog
eClinicalWorks
When taking on risk is the right move
Physicians don’t usually encourage their patients to take unnecessary risks, much less take such risks themselves. After all, they are supposed to be role models. But there are times when taking on risk is not only the right thing to do but can show others the path to a bright healthcare future.
Innova Primary Care of Huntsville, Alabama is an example of a practice that understands when taking on risk is the right move.
For three years, Innova was part of an Accountable Care Organization (ACO) that successfully participated in the Medicare Shared Savings Program (MSSP).
Value-based care: Going beyond the basics
ACOs exemplify the shift from fee-for-service payment models to value-based ones. The name — accountable care — captures the spirit of that shift.
But Innova Primary Care didn’t limit itself to a few Population Health programs and more data analysis. They went further by accepting financial responsibility for the day-to-day costs of care for their patients.
Under downside risk (or two-sided risk), a practice takes on greater responsibility for outcomes and costs — which can mean higher bonuses if they meet their goals. Instead of the 50% savings available under MSSP, an ACO might see 60% or 75% savings.
An invitation to more success — and more data
“Because of our publicly available data, we were invited to shift and join a different ACO,” said David Uptagrafft, Innova’s Chief Financial Officer and Director of Healthcare Experience. “That has resulted in us now transitioning toward an enhanced model ACO which has downside risk. And we’re excited about that because it really changes the way that we’re measured, and it gives us the opportunity to continue succeeding.”
Achieving their goals required having a strong healthcare IT partner with tools capable of helping them meet higher standards.
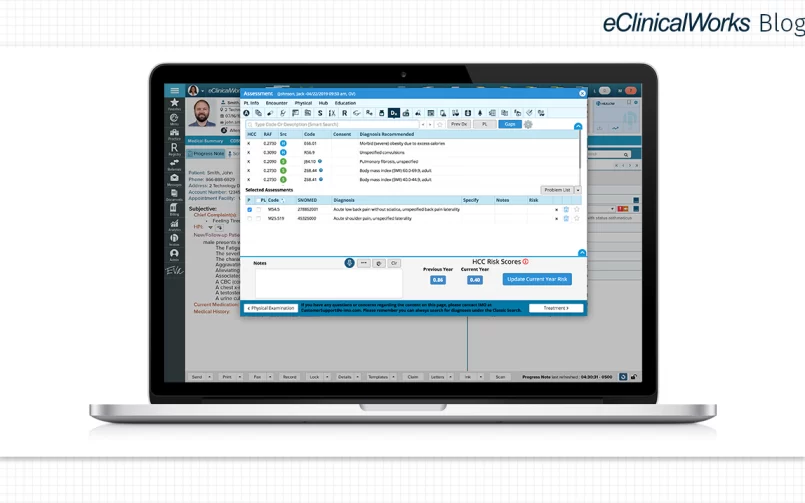
“We track a number of different metrics here for which we utilize eClinicalWorks,” Uptagrafft said. “Two that we publish out front are related to HCC coding. With blood pressure, you can stratify that across all different providers, and we publish that weekly on our screens. Then there’s the data that’s granular — and that has been very valuable — but that we don’t publish all the time. There are some really good eClinicalWorks Business Optimizer reports for Chronic Care Management that tell you which staff member is adding time and what their total time is by the date range you specify.”
How a small practice maintains excellence
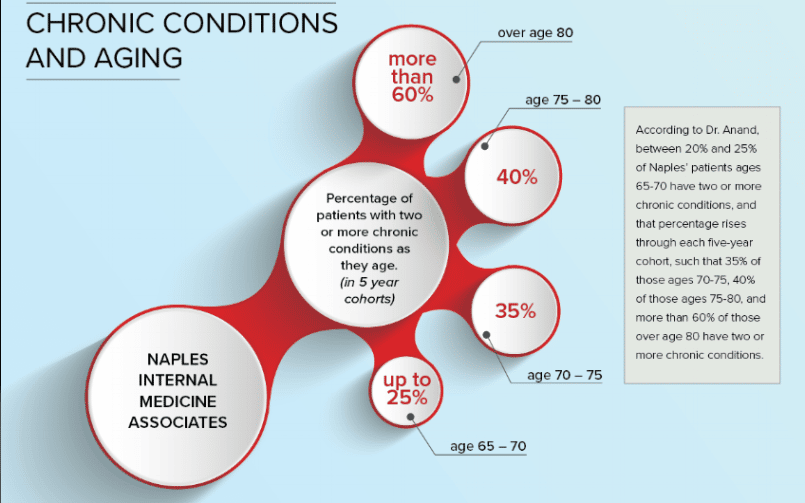
While Population Health tools such as HEDIS®, Hierarchical Condition Category (HCC) coding, and Chronic Care Management can benefit practices of all sizes, Uptagrafft notes that they can dramatically impact a small practice that might be looking for expertise it cannot afford to develop on its own.
“In our case, as an independent, relatively small primary care group, we need these tools,” he said. “We can’t go out and create our own software. We don’t have an internal programming team, and so, the partnership with eClinicalWorks and providing Population Health tools allows us to really outpunch our weight class with regards to performance and quality metrics.”
Having comprehensive and timely data from eClinicalWorks®, Uptagrafft said, means that the practice can continually monitor the performance of its physicians, rather than waiting months for periodic reports that show deficiencies that could and should have been addressed much earlier.
“When we bring in new physicians, one of the best things that we can do is to monitor their risk score coding and see where they are performance-wise,” Uptagrafft said.
In the end, it seems that taking on that additional risk at Innova Primary Care turned out to be just about the safest and best option available.
Get the full story from David Uptagrafft here.
HEDIS is a registered trademark of the National Committee for Quality Assurance (NCQA).