Deriving Greater Value from Telehealth
- 27 April 2020
- Blog
eClinicalWorks

The role of chronic disease management
Although the cost has been high, the coronavirus pandemic has illustrated how much societies around the globe share — and how they can come together to improve health.
The impact of COVID-19 has been severe on those with compromised immunity and pre-existing health conditions, a stark reminder of the toll chronic health conditions take.
According to a study by BMC Health Services Research, nearly two-thirds of deaths worldwide in 2008 were attributable to chronic disease. That means identifying and treating those with chronic illness is a priority during the current pandemic.
Identifying common elements for success
That BMC study, released in May 2015, analyzed 77 studies of chronic care management models in the U.S. and overseas and identified elements of the Wagner chronic care model that can reduce the impact of chronic illness:
- Mobilizing community resources
- Promoting high-quality care
- Enabling patient self-management
- Implementing care consistent with evidence and patient preferences
- Effectively using patient/population data
- Cultural competence, care coordination, and health promotion
CMS introduces Chronic Care Management
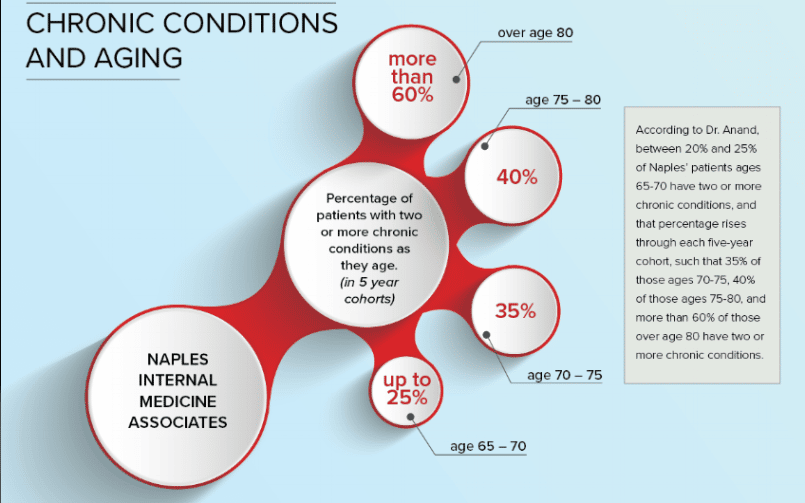
A few months before the BMC study, the Centers for Medicare & Medicaid Services (CMS) introduced its Chronic Care Management program, an effort to improve care for patients with two or more chronic illnesses.
Many practices quickly embraced the CCM program, which offered them a way to be reimbursed for care services they had been providing for years.
CCM is showing success
What has been the impact of the CCM program?
In November 2017, Mathematica Policy Research released a study evaluating the impact of the CCM program over the first two years of its existence, and found that providers and care managers reported:
- Improved patient satisfaction and adherence to therapies
- Greater clinician efficiency
- Fewer hospitalizations and ER visits
The CCM program allows practices to be reimbursed for providing at least 20 minutes of non-face-to-face time each month to patients with two or more chronic conditions.
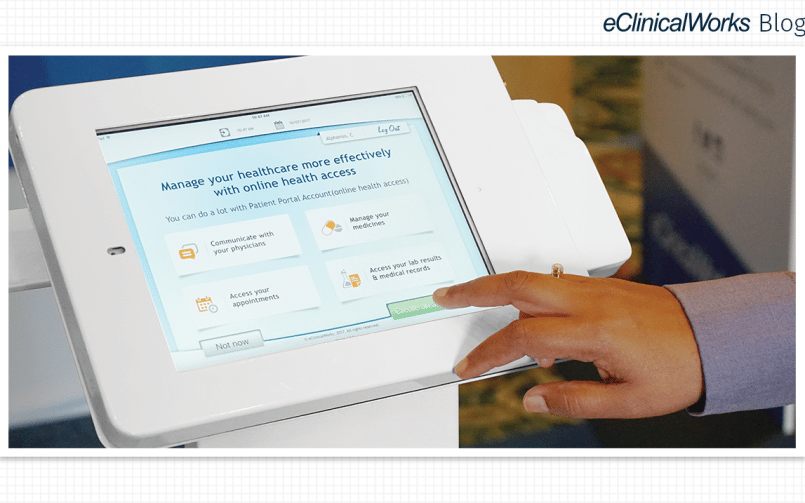
Many eClinicalWorks practices have enabled our CCM solution, part of our suite of Population Health products. eClinicalWorks makes it easy to participate in CCM, with dashboards to identify eligible patients, timers to track the minutes devoted to each patient’s care, and automate generation of claims when the 20-minute threshold is reached.
Three reasons to embrace CCM today
CCM has already demonstrated excellent outcomes for practices around the nation. And there are three key reasons it is particularly timely for providers:
- CCM offers practices a way to reach out to their most vulnerable patients at a time when they need services — and contact with their caregivers — more than ever.
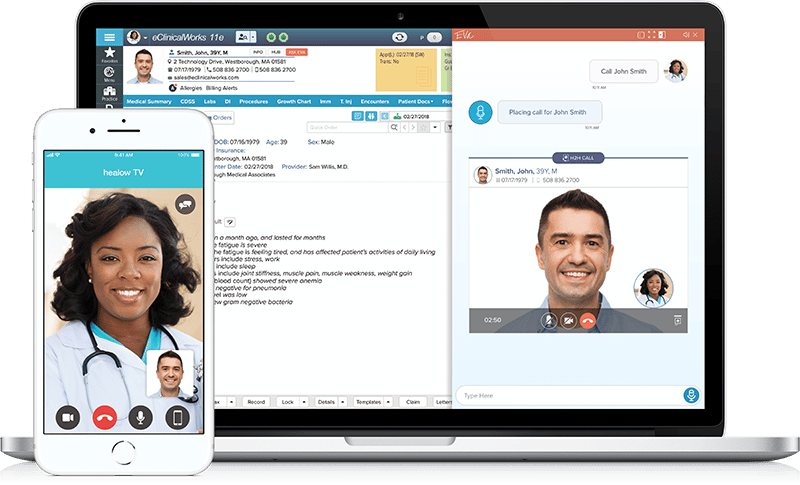
- Our healow Telehealth Solutions, including healow TeleVisits™ and hello2healow™, offer practices affordable and convenient ways to conduct the audio/visual calls that qualify toward the 20-minute monthly requirements of the CCM program.
- With so many practices forced to curtail physical office visits, combining telehealth technology with the CCM program is an effective way to claim reimbursements for services medical practices are already providing — at a time when revenues may be reduced.
Related Post

- 9 January 2025
- Blog
Unveiling Trends Set to Transform Healthcare in 2025

- 15 February 2024
- Blog
AI Medical Scribes in Remote Healthcare Services

- 7 November 2023
- Blog
Embracing Technology for Startup Weight Loss and Medical Spa Clinics
- 27 September 2022
- Blog
Back to School — for Your Practice, Too!

- 17 August 2022
- Blog
Addressing the Acute Need for Chronic Care Services

- 21 June 2022
- Blog
Dermatology Made Easier This Summer

- 25 March 2022
- Blog
HIMSS22 Outlines Opportunities in Healthcare

- 17 February 2022
- Blog
Defense Matters: Keeping Remote Medicine Safe

- 10 February 2022
- Blog
All the Ingredients for Population Health Management

- 1 February 2022
- Blog
One Key for 2022: Staying Focused on Patients
- 28 January 2022
- Blog
4 Patient Engagement Solutions to Help Patients and Practices in 2022
- 25 January 2022
- Blog
The Right Tools During Challenging Times

- 19 January 2022
- Blog
Healthcare 2022: Regulatory Trends to Look for in the Year Ahead

- 28 December 2021
- Blog
Looking Back at 5 Key Success Stories from 2021
- 18 November 2021
- Blog
Remaining Vigilant in the Lung Cancer Fight
- 4 November 2021
- Blog
Telehealth Is Long-Established Science Fact
- 2 November 2021
- Blog
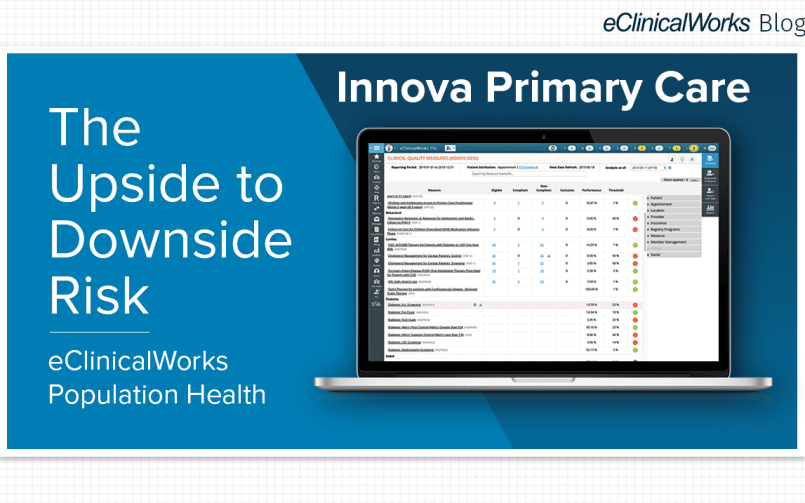
Innova Primary Care: The Upside to Downside Risk
- 2 September 2021
- Blog
It’s Time for a Better Check-in Solution
- 12 August 2021
- Blog
Using hello2healow for Patient Outreach in Florida
- 27 May 2021
- Blog
When Neurological Care Cannot Wait

- 20 May 2021
- Blog
Solutions for Allergy Testing, Tracking, and Treatment

- 16 March 2021
- Blog
A Partner for Reinventing Your Practice
- 2 March 2021
- Blog
What it Takes to Better Know Your Patients

- 29 January 2021
- Blog
Putting the Pieces Together for Quality Healthcare
- 30 December 2020
- Blog
2020 eClinicalWorks Year in Review
- 22 December 2020
- Blog
Thirlby Clinic: Using Telehealth and CCM for Better Disease Management

- 15 December 2020
- Blog
A Challenging Year Is Ending — New Opportunities Ahead

- 10 December 2020
- Blog
How a Practice Found Success With Telehealth & Contactless Check-In
- 24 November 2020
- Blog
The Continuing Influence of Telehealth
- 19 November 2020
- Blog
Meeting the Demand for Behavioral Health Services

- 12 November 2020
- Blog
Reinventing Healthcare for a Brighter Future
- 6 November 2020
- Blog
How Little River Medical Center Thrived During the Pandemic
- 19 October 2020
- Blog
How Telehealth, CCM, and Contactless Check-In Revitalized a Practice in Need

- 15 October 2020
- Blog
Targeting Behavioral Health, Remote Care & More
- 30 September 2020
- Blog
Surviving COVID-19: Telehealth and Beyond
- 21 September 2020
- Blog
3 Important healow TeleVisits Features
- 9 September 2020
- Blog
It’s Your Practice — Dream Big!
- 1 September 2020
- Blog
Back to the Basics During the COVID-19 Era
- 28 August 2020
- Blog
How the Patient Portal Is Making a Difference for a Pediatric Practice
- 7 August 2020
- Blog
Back to the Basics: Population Health

- 24 July 2020
- Blog
Pushing Boundaries, Reaching New Horizons

- 17 July 2020
- Blog
How to Keep Your Patients & Staff Safe During COVID-19
- 13 July 2020
- Blog
The Importance of Chronic Care Management Today
- 1 July 2020
- Blog
How to Digitize Your Front Office

- 29 June 2020
- Blog
The Telehealth Revolution Continues
- 24 June 2020
- Blog
How Advocare Put healow TeleVisits™ to Work
- 17 June 2020
- Blog
How Telehealth Is Connecting Patients & Providers

- 12 June 2020
- Blog
Finding a New Normal: The Patient Experience
- 10 June 2020
- Blog
Minding Mental Health During COVID-19
- 3 June 2020
- Blog
Expanding the Range of Specialty Care

- 1 June 2020
- Blog
Reinventing Your Practice

- 29 May 2020
- Blog
What Telehealth Could Mean for Practices Today

- 27 May 2020
- Blog
Resourceful Action During Extreme Times

- 21 May 2020
- Blog
Like Telehealth? There’s More!
- 19 May 2020
- Blog
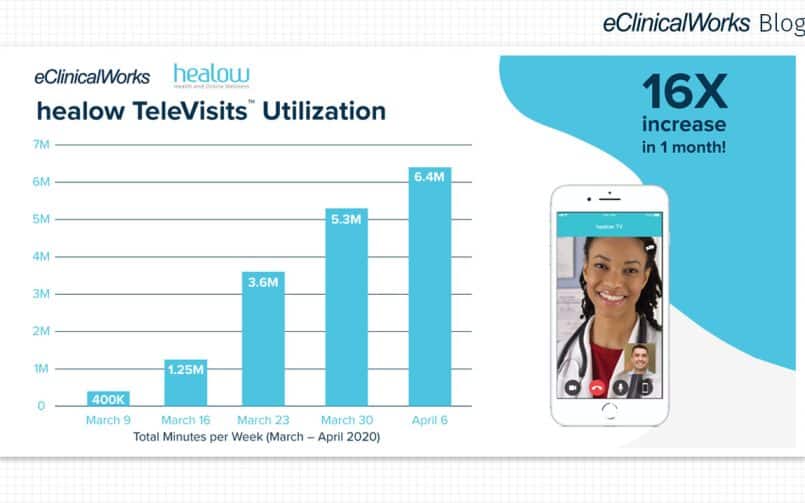
The Numbers Behind TeleVisits

- 16 May 2020
- Blog
What Telehealth Can Do for Specialty Practices

- 13 May 2020
- Blog
Routine Care During Nonroutine Times

- 12 May 2020
- Blog
How Telehealth Will Make The 21st Century Ours

- 8 May 2020
- Blog
Seeing Medicine in a New Light

- 7 May 2020
- Blog
Telehealth: Healing Action at a Distance

- 5 May 2020
- Blog
3 Patient Stories of TeleVisits in Action

- 1 May 2020
- Blog
Sustaining Medical Practice During COVID-19
- 29 April 2020
- Blog
The Evolution and Importance of Telehealth

- 24 April 2020
- Blog
3 Practices Finding Success With Telehealth

- 22 April 2020
- Blog
How Innovation Fueled the Rise of Telehealth

- 20 April 2020
- Blog
Why You Should Activate Telehealth Today

- 17 April 2020
- Blog
3 Practices Using Telehealth to Improve Patient Care

- 15 April 2020
- Blog
Shift in the Medical Mindset
- 13 April 2020
- Blog
How Telehealth Kept a Patient Out of the ER

- 10 April 2020
- Blog
Speeding Toward a New Healthcare Paradigm

- 9 April 2020
- Blog
How Dallas Renal Group is Providing Care While Social Distancing

- 8 April 2020
- Blog
Swift Action Results in Change of Telehealth Regulations

- 7 April 2020
- Blog
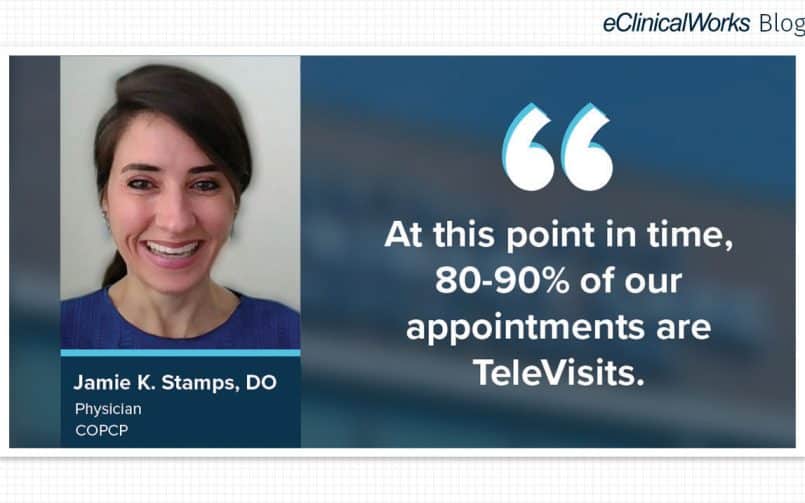
How Central Ohio Primary Care Physicians is Reducing ER Visits
- 6 April 2020
- Blog
Securing Access to Care During a Pandemic

- 3 April 2020
- Blog
How Telehealth is Keeping Patients Safe at Trusted Doctors

- 2 April 2020
- Blog
Flattening the Curve With Telehealth
- 1 April 2020
- Blog
How First Choice Neurology Transformed Their Practice With Telehealth

- 31 March 2020
- Blog
Telehealth and Mental Health in a Time of Crisis
- 27 March 2020
- Blog
How SG Pediatrics are Using TeleVisits to Help Patients
- 26 March 2020
- Blog
The eClinicalWorks Telehealth Advantage
- 25 March 2020
- Blog
How Televisits Have Transformed Comprehensive Sleep Center

- 24 March 2020
- Blog
Telehealth: Helping Throughout History
- 23 March 2020
- Blog
How healow TeleVisits Can Help During a Health Crisis
- 20 March 2020
- Blog
healow TeleVisits: How Fast Deployment Helps
- 11 March 2020
- Blog
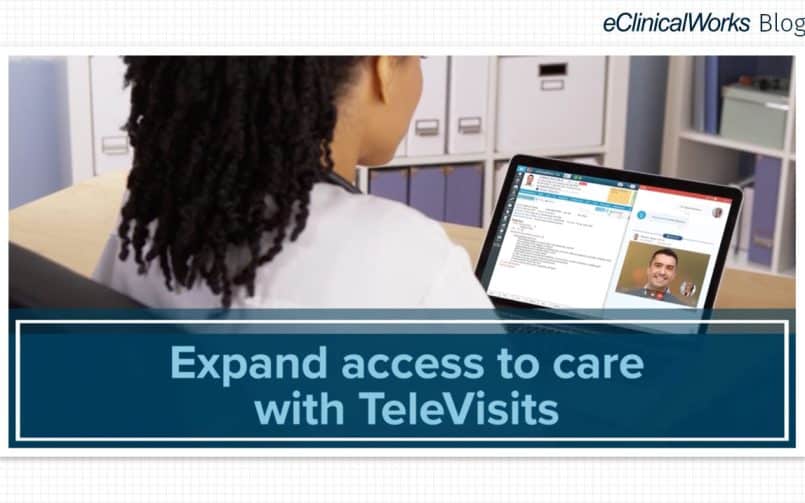
Expanding Access to Care With healow TeleVisits
- 17 January 2020
- Blog
Teledentistry: Expanding Access to Dental Care
- 8 January 2020
- Blog
The State of Telehealth in 2020
- 14 August 2019
- Blog
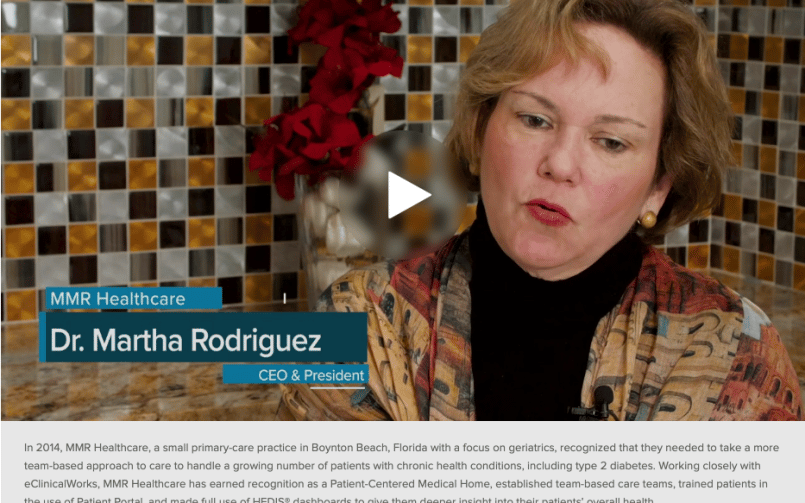
Patient-Centered Care: How the Approach Can Improve Healthcare

- 5 June 2019
- Blog
3 Ways That Telehealth Is Improving Healthcare
- 21 March 2019
- Blog
CCM: A Long-term Commitment to Teamwork
- 9 January 2019
- Blog
Telehealth – Rural Health Center

- 1 November 2018
- Blog
Three Ways Telemedicine Improves Care for Providers and Patients

- 15 October 2018
- Blog
How telehealth helps to improve compliance among ADHD patients

- 7 October 2018
- Blog
Powering Through on Game Day!

- 6 October 2018
- Blog
Making Connections on Saturday
- 30 May 2018
- Blog
ADHD and Telemedicine: A Natural Fit
- 21 August 2017
- Blog
Brown Clinic: Superusers Building Value
- 26 June 2017
- Blog
Chronic Care Management: Improving Quality of Care
- 19 June 2017
- Blog
Chronic Care Management and Aging
- 20 March 2015
- Blog
The Next Phase of Innovation in Healthcare
- 20 March 2015
- Blog