3 Ways to Change Unproductive Touches in Your Revenue Cycle
- 7 November 2024
- Blog
Waystar
This blog is presented by Waystar as part of their sponsorship of the 2024 eClinicalWorks® and healow® National Conference.

Many things affect the healthcare revenue cycle today. Ever-changing payer rules and insufficient edits. Staffing challenges. Time wasted on fruitless tasks (like statusing claims).
“All of that leads to poor utilization of limited staff and a frustrating result: You keep trying to dig yourself out of a hole only to end up digging a deeper one,” says Christine Fontaine, Waystar Solution Strategist.
Finding ways to eliminate unproductive work in Revenue Cycle Management (RCM) is one very important way hospitals, health systems, and providers can make a difference.
“I’ve worked with many organizations that, after investigating their processes, found that they’re losing productivity because staff is managing work that could easily be automated,” says Fontaine. “I call these unproductive touches, and I see a few over and over again.”
So, how do you put a stop to wasted effort and improve your healthcare RCM processes? Here are three areas in your organization where you can look for easy improvement:
- Insurance verification + coverage detection
- Claim statusing
- Denial + appeal management
1. Insurance verification + coverage detection
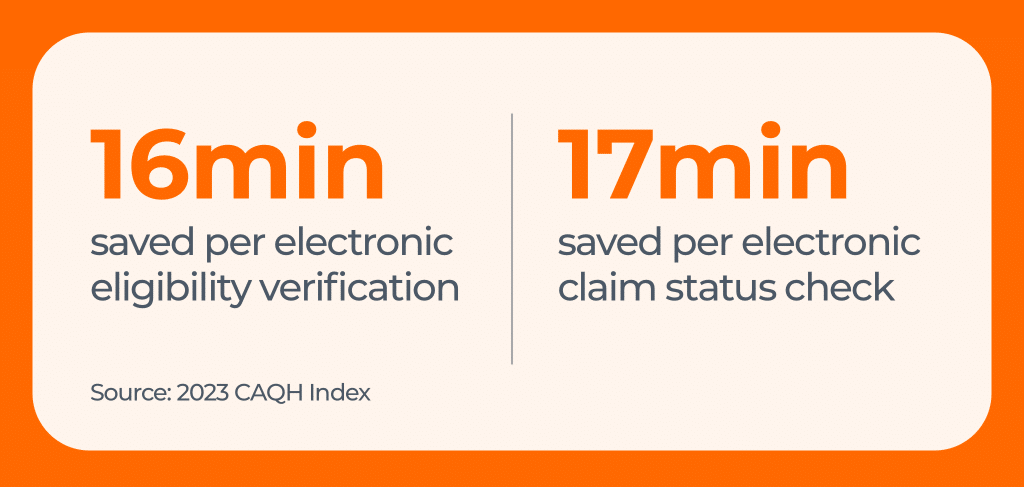
Manually verifying eligibility and looking for coverage adds cost and time to each transaction, which contributes to staff inefficiency. In fact, professionals who verify eligibility manually waste 16 minutes of time per transaction compared with those who use electronic eligibility verification, according to the 2023 CAQH Index. The industry could save $9.3 billion each year by automating this process.
“Some organizations report their staff spends more than two hours per day just following up with payers! So, it’s easy to see how the industry as a whole could save billions with automation,” Fontaine says.
Additionally, some patients assume they don’t have billable coverage when in fact, they do. For example, Waystar, a healthcare RCM software company, offers a tool that finds hidden coverage for 30 to 40% of presumed self-pay patients.
To remove this unproductive touch from your organization’s processes, look for automated insurance eligibility and coverage software that:
- Identifies hidden coverage
- Uses AI + robotic process automation (RPA) to augment missing data from X12
- Accesses vast amounts of payer data to curate accurate benefit information
- Offers robust alerts so teams can work by exception
- Triages eligibility issues so staff can prioritize tasks properly
- Seamlessly integrates with your EHR
Ready for the coverage changes that come with open enrollment? Check out this webinar to learn how to craft a plan now to ensure your team can catch insurance changes and find hidden coverage on January 1.
2. Claim statusing
One revealing question for every RCM leader is:
How much time does it take for your team to resubmit a claim or create an appeal?
If your staff is making calls and checking websites, then the answer is: “Too much.”
“Retrieving actionable information from payers about claim status is very time consuming and it often results in needlessly touching claims that are already being processed properly,” Fontaine says. “That takes staff away from higher value tasks, such as working problem claims.”
To address that, providers are leveraging RPA to save time and money, in addition to improving staff satisfaction. Seventeen minutes can be saved per claim status check when using smart claim status software versus doing the process manually.
“Automation leads to less human error, wasted efforts, re-work, and staff friction,” says Fontaine.
Forbes backs that up, reporting that a poll by Tech.co found that 59% of employees say AI has improved their job satisfaction. With automation and AI, employees are more engaged and satisfied when they can focus on meaningful, useful tasks.
If claim statusing is an unproductive touch in your organization, look for an automated solution that:
- Predicts the right time to status a claim and intelligently drives follow-up
- Facilitates rapid intervention using flexible payer connections
- Curates the most enriched status response
- Controls status checks with a scheduling capability
- Proactively monitors payer portals
Looking to simplify claim statusing and other claim management processes? Download this eBook: Achieve claim management clarity with these 4 strategies.
3. Denial + appeal management
The KFF Survey of Consumer Experiences with Health Insurance found that 18% of insured adults say they experienced denied claims in the past year. And it’s very expensive for healthcare organizations to overturn them. Hospitals and health systems spend an estimated $19.7 billion in one year trying to overturn denied claims, according to the American Hospital Association. The costs are high in part because manually gathering information and creating and submitting appeals saps hours of staff time every week.
Automation is a highly effective way to reduce denials and boost margins, especially when combined with analytics that give staff actionable information. For example, advanced solutions can help staff identify accounts with the highest likelihood of success, so they know which appeals to work first.
If your staff spends too much time working a growing volume of appeals, look for an automated solution that:
- Triages denials based on probability of success
- Automatically routes denials to appropriate teams or work queues
- Provide real-time, one-click eligibility verification
- Offers pre-populated payer-specific forms to auto-generate appeals
- Automatically submits paperless appeals packages directly to payers
If denials are draining your staff’s time, get the Denial prevention playbook: 11 top causes of denials (and how to fix them). You’ll get a detailed look at the top denials — along with strategies to resolve, prevent, and automate related tasks in the future.
“There’s no doubt it’s a challenging time to be in revenue cycle management,” says Fontaine. “But it’s also an exciting time because there are so many opportunities to use automation to increase efficiency and help your staff engage while increasing their satisfaction.”